7.Iron,Minerals and Trace Elements
METHODS
Literature Search
Timeframe:1990–2004,in addition relevant earlier pub-lications were considered.
Type of publications:randomised controlled studies;case-control or cohort studies;case reports;case series;expert opinion.
Key Words:calcium,chromium,copper,iodine,iron, manganese,magnesium,molybdenum,newborn,parenteral nutrition,phosphorus,selenium,trace elements,zinc. Language:English.
IRON
Introduction
Iron is not routinely provided in parenteral nutrition mixtures and is often not a component of commercially available trace element preparations.Currently there are no well-de?ned recommendations regarding the opti-mum content of iron in parenteral feeds,and intravenous administration of iron remains problematic.One major concern is that of iron overload.Parenteral administra-tion of iron bypasses the homeostatic control of gas-trointestinal iron absorption,causing loss of protection from iron overload if excessive quantities are provided. An accumulation of excess iron has been reported in children receiving prolonged parenteral nutrition.In a study of30children aged1–18years receiving ferrous sulphate100m g/kg per day for an average period of 43months,12children showed evidence of plasma and hepatic iron overload.Ferritin concentrations were .800ng/ml in eight children(.1100ng/ml in?ve)and correlated with duration of PN.The degree of iron de-position in either hepatocytes or Kupffer cells was most pronounced in children with the higher ferritin concen-trations((1)(LOE2+)).Thus,iron status of children receiving long-term PN should be monitored by regular measurement of serum ferritin,and supplementation decreased if ferritin concentration is raised.Although Ben-Hariz et al suggested halving iron intake at ferritin concentrations of500ng/ml and stopping completely at 1000ng/ml,these concentrations probably leave only a small margin of safety.There is,therefore,an argument for curtailing iron supplementation at lower plasma ferritin concentration.
A further concern over parenteral iron administration is that it may impair immune function and stimulate bacterial growth thus increasing the risk of infection by iron-requiring pathogens(2).Iron availability correlates with bacterial growth and virulence,facilitates viral rep-lication and reverses the bactericidal effect of lactoferrin and lysozyme(3,4).Furthermore,the antibacterial effect of cytokines is mediated by intracellular iron depletion. Interferon,IL-1,and tumour necrosis factor enhance ferritin synthesis resulting in a shift of cellular iron into a storage compartment and downregulate transferrin receptor production decreasing cellular iron uptake and, thereby,iron availability for intracellular pathogens(5). Iron therapy has also been implicated in decreased phagocytosis and inhibition of CD4and CD8helper T cell proliferation while enhancing the function of sup-pressor T cells(6).Yet,several components of the immune response are depressed in iron de?ciency.An impaired capacity for the generation of the oxidative burst has been observed in phagocytes from iron de?cient children(7).McFarlane et al studied40children with kwashiorkor and low serum transferrin given nutritional support including iron supplements.Many of the children who received iron therapy died shortly after supplements were begun suggesting that provision of iron in a setting of low transferrin may have resulted in higher circulating free iron that could have contributed to the development of overwhelming infection and death(8).Septicaemia with Yersinia enterocolitica has been reported in healthy children overdosed with oral iron(9).Nevertheless,there is little clinical evidence that iron supplementation in parenterally fed children increases the risk of sepsis(10). Adverse drug reactions associated with parenteral iron therapy are common,although side effects are mild and self limiting((11,12)(LOE2+)).In various series2–5% of patients experience signi?cant side effects.The pro-cesses leading to iron dextran induced symptoms are unclear,but include a type I(IgE-mediated)anaphylactic reaction which is caused by preformed dextran anti-bodies.Additional mechanisms include a type I anaphy-lactoid reaction that may be caused by transient overload of the transferrin molecule resulting in small amounts of free iron in the circulation(which appears to be dose related)and immune complex activation by speci?c IgG antibody.Symptoms include dyspnoea,wheezing,hypo-tension,nausea,vomiting,abdominal pain,arthralgia and myalgia.Most side-effects are mild and self-limiting with severe reactions occurring in a minority of patients and in conjunction with infusion of larger iron doses.An increased incidence of adverse effects has been reported in patients with collagen diseases.Despite previous
Journal of Pediatric Gastroenterology and Nutrition
41:S39–S46óNovember2005ESPGHAN.Reprinted with permission.
S39
episodes of allergic reactions safe administration of iron dextran is possible following a pre-treatment protocol of methylprednisolone,diphenydramine and ephedrine. While total dose infusions of iron dextran may be asso-ciated with allergic manifestations the administration of the standard maintenance doses(estimated at1–2mg/day up to10–15mg/day)may be well tolerated(11,13). There is a paucity of studies on the effects and complications of intravenous iron in children.No adverse effects were reported in14children who received 15mg/kg of iron dextran during a two hour period(13), in2children who received IV iron at a dose of250–500mg at an infusion rate of a100mg/min(14),or in 5premature infants given iron dextran at a dose of10–450m g/kg per day(15).Similarly,no complications were observed in a study of14very low birth weight infants receiving IV iron supplementation at a dose of200–250m g/kg per day((16)(LOE1+)).
The ability of iron both as Fe3+(bound form)or Fe2+ (free iron)to generate free oxygen radicals has also raised concerns regarding safety.In addition,parenteral lipid emulsion also generates peroxides(17).The rich content of double bonds of the lipid emulsion makes it a good substrate for iron-induced peroxidation.Light in-duced generation of peroxides in PN solutions and the interaction of iron complexes(iron dextran)with photons or substrates of photo-oxidation,such as vitamins or polysorbate,could explain the unexpected observation that bound iron is protective against spontaneous per-oxide generation in PN solutions(18).
The compatibility of iron with PN solutions has not been clearly established.Iron dextran cannot be added to lipid emulsions or all-in-one mixes as it results in destabilisation of the https://www.doczj.com/doc/c24302467.html,patibility of iron dextran has been shown in amino acid-glucose solutions for up to18hours(19).Ferrous citrate is also compatible with PN solutions,with no observed precipitation during infusion periods of18–24hours(20).
Whether or not there is a need for routine iron supplementation of PN remains controversial.A special concern is the low birth weight infant because of possible increased risk of infection observed following intra-muscular iron(21).Arguments in favour of iron sup-plementation in VLBW infants include their low iron stores,rapid growth rate,increased requirements for iron when erythropoesis resumes at approximately2months of age,and caution required in relation to repeated blood transfusion.It has been estimated that these newborns need700to1000m g/kg per day to reach iron balance (15,16)although considerably lower doses may suf?ce ((22)(LOE4));possibly erythropoeitin is needed to use the iron administered.In term infants receiving PN it is estimated that the daily parenteral iron requirement is 100m g/kg per day(22).Although iron reserves should be adequate to supply red cell production for3–5months, iron de?ciency has been shown to develop much sooner. How early parenteral iron supplements should be commenced in infants and children receiving PN will depend on the underlying pathology and degree of blood loss.In short term PN of a few weeks no adverse effects resulting from lack of iron supplementation have been observed(10).During long-term PN the child’s iron status should be monitored closely and supplementation begun as soon as impending de?ciency is identi?ed.
In summary,iron supplementation with iron dextran added to amino acid-glucose solutions can be safely ad-ministered at maintenance doses.Preterm infants require parenteral iron but may also require erythropoietin for utilisation.Term infants and older children probably do not need iron supplementation when receiving short-term PN. Timing the initiation of iron supplementation in the diverse population of children requiring PN should be based on their underlying morbidity,previous surgical interventions and potential blood losses.In children receiving parenteral iron supplementation close monitoring of iron status is mandatory to avoid iron overload.
TRACE ELEMENTS
Introduction
Chromium,copper,iodine,manganese,molybdenum, selenium and zinc are essential micronutrients involved in many metabolic processes.Parenteral nutrition aims to meet nutritional needs while avoiding complications; precise requirements for individual nutrients remain a matter of debate((23)(LOE2+)).Trace elements are involved in enzymatic activities and immunologic
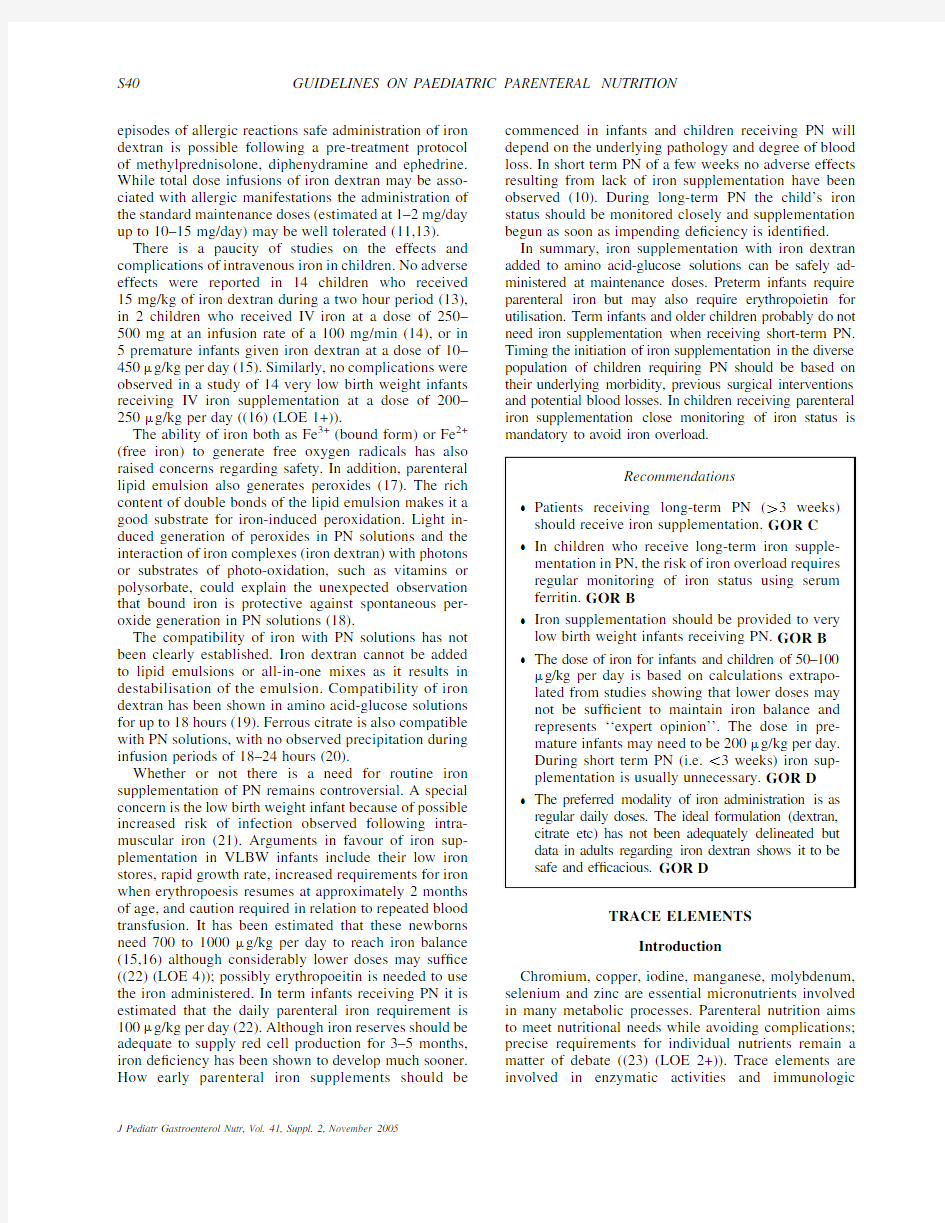
Recommendations
Patients receiving long-term PN(.3weeks)
should receive iron supplementation.GOR C
In children who receive long-term iron supple-
mentation in PN,the risk of iron overload requires
regular monitoring of iron status using serum
ferritin.GOR B
Iron supplementation should be provided to very
low birth weight infants receiving PN.GOR B
The dose of iron for infants and children of50–100
m g/kg per day is based on calculations extrapo-
lated from studies showing that lower doses may
not be suf?cient to maintain iron balance and
represents‘‘expert opinion’’.The dose in pre-
mature infants may need to be200m g/kg per day.
During short term PN(i.e.,3weeks)iron sup-
plementation is usually unnecessary.GOR D
The preferred modality of iron administration is as
regular daily doses.The ideal formulation(dextran,
citrate etc)has not been adequately delineated but
data in adults regarding iron dextran shows it to be
safe and ef?cacious.GOR D
S40GUIDELINES ON PAEDIATRIC PARENTERAL NUTRITION J Pediatr Gastroenterol Nutr,Vol.41,Suppl.2,November2005
reactions.Although toxicity is infrequent,it is well described in patients receiving PN((24)(LOE2+)).Low-birth-weight infants(LBW)are at risk of trace element de?ciency both because they are born before adequate stores can be acquired and because of the demands of their rapid growth((25)(LOE2++);(26)).Parenteral mineral and trace element delivery are calculated to prevent the development of de?ciency syndromes ((27)(LOE2+))and to match in-utero accretion rates ((28)(LOE2+)).Parenteral solutions are contaminated with metals such as aluminium and chromium;these require monitoring during long-term PN((29)(LOE2+)).
A change from glass to plastic packaging for PN products may have implications for trace element supplementation through decreased contamination.Trace element status should be closely monitored in cholestatic patients and trace element preparations may need to be discontinued to avoid copper toxicity.Patients with renal impairment may not be able to excrete selenium,molybdenum,zinc and chromium((29,22)(LOE1+)).When taking blood sam-ples for trace element analysis it is important to avoid contamination of the specimen.
Chromium
Chromium(Cr)is an essential micronutrient required for carbohydrate and lipid metabolism.Cr de?ciency has been described in patients receiving long-term PN,but patients receiving PN also have been reported to show increased serum Cr level((30)(LOE2+)).Efforts are required to?nd PN components with low or,if possible, no Cr contamination(30).High serum Cr competes with iron for binding to transferrin and,hence negatively in-terferes with iron metabolism and storage((31)(LOE3)).
A daily intake of0.2m g/kg per day has been recom-mended for infants and children(maximum of5m g/day) receiving PN((22)(LOE2++)),although there is some evidence that lower intakes would be adequate((32)(LOE 2+)).Supplementation is unnecessary since Cr contam-inates PN solutions to a degree that satis?es requirements ((33)(LOE2+)).
Copper
Copper(Cu)is a component of several enzymes,in-cluding cytochrome oxidase,superoxide dismutase(Cu/Zn SOD),monoamine oxidase and lysyl oxidase.Copper concentrations in plasma and cells as well as copper metalloenzymes are indicative of copper status((34,35) (LOE2++)).Monitoring plasma concentration of both Cu and caeruloplasmin,the major Cu transport protein, should be considered during PN((36)(LOE2+)).How-ever,superoxide dismutase(SOD)activity in erythro-cytes seems to be a more sensitive indicator of Cu de?ciency than plasma concentration of Cu or caerulo-plasmin((37)(LOE2++)).Other indicators of Cu status include neutrophil counts(low in de?ciency),SOD ac-tivity,platelet cytochrome-c oxidase activity and platelet copper concentration((35)(LOE2++)).Cu should be carefully monitored in patients with cholestatic liver dis-ease((22,38)(LOE2++)).
Plasma total Cu and caeruloplasmin are invariably reduced in children with burns((36)(LOE2+)).PN in these patients must be supplemented with more than 20m g/kg Cu to avoid de?ciency((39)(LOE2+)).The high Cu content in gastrointestinal?uid means that losses should be balanced by a higher Cu intake(increased by 10–15m g/kg)in PN(22).A routine intravenous supply of20m g/kg per day copper for infants(preterm and term) and children is recommended((22)(LOE2++)).
Iodine
Iodine is an essential part of the thyroid hormones, thyroxin(T4)and tri-iodothyronine(T3),which are nec-essary for cellular metabolism and maintenance of meta-bolic rate.Thyroid function remained normal and serum iodine levels were not reduced in children receiving long-term PN without iodide supplementation,probably due to iodine contamination of the solutions and skin absorption of topical iodinated disinfectant((40)(LOE 2+)).It is also possible in these patients that there was some absorption of iodine present in the ingested food. However,a daily dosage of1m g/d is recommended for infants and children receiving PN((22)(LOE2++)).Now
Recommendations
Trace elements should be supplied with long-term parenteral nutrition.GOR D
Trace elements should be periodically monitored in patients on long-term parenteral nutrition.
GOR D
Recommendation
Cr contaminates PN solutions to a degree that sat-is?es requirements,therefore,additional supple-mentation of Cr is considered unnecessary.GOR C
Recommendations
Parenterally fed infants and children should receive an intravenous supply of20m g/kg per day copper.GOR D
Plasma copper and caeruloplasmin concentra-tions should be monitored in patients receiv-ing long term PN and in parenterally fed patients with burns or with cholestasis,and adjustment of copper supply be considered accordingly.GOR D
GUIDELINES ON PAEDIATRIC PARENTERAL NUTRITION S41
J Pediatr Gastroenterol Nutr,Vol.41,Suppl.2,November2005
that use of iodine for skin cleaning is relatively un-common,there may need to be a reassessment of iodine requirements.
Manganese
Manganese(Mn)is a component of several enzymes including mitochondrial superoxide dismutase and also activates other enzymes such as hydrolases,kinases and transferases.High Mn intake during PN is probably one of several factors contributing to the pathogenesis of PN associated cholestasis or other hepatic dysfunction ((41)(LOE3);(38)(LOE2++);(42)(LOE2++);(43) (LOE1)).Mn should,therefore,be carefully adminis-tered,particularly in patients receiving long-term PN ((38)(LOE2++);(44)(LOE3);(45)(LOE2+)).Studies using magnetic resonance images(MRI)have reported high-intensity areas in basal ganglia,thalamus,brainstem and cerebellum due to Mn intoxication with disappear-ance of symptoms and MRI abnormalities after with-drawal of manganese administration((46)(LOE2+);(47) (LOE3);(48)(LOE3);(44)(LOE3)).As central nervous system deposition of Mn can occur without symptoms,regular monitoring of manganese blood concentration should be performed in children on long-term PN.Taking into account the hazards of high Mn levels in children receiving long-term PN,a low dose regimen of no more than1.0m g(0.018m mol)/kg per day (maximum of50m g/d for children)is recommended ((22,38)(LOE2++))together with regular examination of the nervous system(38).
Molybdenum
Molybdenum(Mo)is essential for several enzymes involved in the metabolism of DNA.To our knowledge there are no reports of Mo de?ciency in infants.However, low-birth-weight infants(LBW)might be at particular risk for Mo de?ciency((49)(LOE2+)).Excess of Mo interferes with Cu metabolism.According to some authors an intravenous intake of1m g/kg per day(0.01m mol/kg per day)seems to be adequate for the LBW infant ((49)(LOE2+)).0.25m g/kg per day is recommended for infants and children(to a maximum of5.0m g/day) ((22)(LOE2++)).Intravenous Mo supplements are rec-ommended only with long-term PN.
Selenium
Selenium(Se)acts as an antioxidant by being an essential component of active glutathione peroxidase (GSHPx),an enzyme that may protect against oxidative tissue damage.Oxidative injury,particularly in the?rst days of life,is associated with long-term complications of prematurity((50)(LOE2++)).Low Se status has been documented in pre-term infants and has been implicated in oxidative diseases such as bronchopulmonary dyspla-sia and retinopathy of prematurity((51)(LOE3);(50) (LOE2++)).Tissue concentrations of Se and activities of selenium-dependent glutathione peroxidase(Se-GSHPx) are useful indicators of Se status((52)(LOE2+)).In order to identify Se de?ciency in children receiving PN,it has been recommended that plasma and red cell selenium concentration and Se-GSHPx are monitored((53)(LOE3)). Erythrocyte and platelet GSHPx activity are sensitive indexes of Se status in PN patients((54)(LOE2+);(55) (LOE2++)).
Several authors have cautioned against high doses of selenium supplementation because of the risk of toxicity. However there have been no reports of selenium toxicity in infants.Se is also known to be important in thyroid metabolism but selenium de?ciency does not seem to play a major role in neonatal hypothyroidism((56)(LOE 2++)).A non-speci?c myopathy has also been associated with Se de?ciency on long-term home PN((57)(LOE3)).
A dose of2–3m g/kg per day has been recommended for LBW infants,although the optimal form and dose remain unclear((22)(LOE2++);(58)(LOE2++);(56)(LOE 2++)).It should be kept in mind that Se supplementation may also affect copper metabolism((59)(LOE1)).
Se content in mature breast milk ranges from6–28m g/L in the USA and Europe(52)representing an average intake of around2.5m g/kg per day with perhaps an80%absorption.Serum Se concentration is lower in
Recommendation
Parenterally fed infants and children should receive a daily iodine supply of1m g/d.GOR D
Recommendation
In children receiving long-term PN,a low dose supply of no more than1.0m g(0.018m mol)/kg per day(maximum of50m g/d for children)is recommended.GOR D
Recommendations
An intravenous molybdenum supply of1m g/kg per day(0.01m mol/kg per day)seems adequate and is recommended for the LBW infant.GOR D For infants and children an intravenous molybde-num supply of0.25m g/kg per day(up to a max-imum of5.0m g/day)is recommended.GOR D
S42GUIDELINES ON PAEDIATRIC PARENTERAL NUTRITION J Pediatr Gastroenterol Nutr,Vol.41,Suppl.2,November2005
PN fed infants than those who are enterally fed with either formula or mother’s milk using current recom-mended intakes((60)(LOE2++)).Premature infants (particularly the very low birth weight)might require double the currently recommended Se intake of1–3m g/kg per day.Selenite is retained better than selenate,although it has a more variable absorption.The organic compound selenomethionine is chemically stable and well retained by the body and can be used in parenteral nutrition.
Zinc
Zinc(Zn)is involved in the metabolism of energy, proteins,carbohydrates,lipids and nucleic acids and is an essential element for tissue accretion.Urinary Zn ex-cretion occurs in the parenterally fed infant.Some amino-acids like histidine,threonine,and lysine have been shown to bind Zn increasing its renal ultra-?lterability((61)(LOE2+)).Increased urinary losses of Zn and decreased plasma concentrations occur following thermal injury in children((39)(LOE2+)).Premature infants need a higher zinc intake than term infants because of their rapid growth:450–500m g/kg per day to match in-utero accretion rate((62)(LOE2+)).Standard trace element preparations do not supply this amount, and additional zinc(zinc sulphate)may need to be added to PN?uid in the preterm infant,or those patients with high zinc losses e.g.from diarrhoea,stomal losses or severe skin disease((63)(LOE2+)).Recommendations are for an intravenous intake of250m g/kg per day and 100m g/kg per day respectively for infants less or more than3months of age,and50m g/kg per day for children (maximum of5.0mg/day)((22)(LOE2++)).Zn is the only trace element that should be added to solutions of patients on short-term PN(22).
CALCIUM,PHOSPHORUS AND MAGNESIUM
Introduction
The requirements of calcium(Ca)and phosphorus(P) are considered together because the majority of both elements are found together as components of the bone mineral apatite[Ca5(PO4)3OH].97%of whole body Ca is stored in apatite together with80%of whole body P(64,65).The molar Ca:P ratio is1.3in the whole body and1.67in apatite.Serum calcium exists in three frac-tions:ionised calcium(approximately50%),protein-bound calcium(approximately40%),and a small amount of calcium that is complexed,primarily to citrate and phosphate ions.Serum calcium is maintained at a con-stant level by the actions of several hormones,most notably parathyroid hormone and calcitonin.Calcium absorption is by the passive vitamin D-independent route or by the active vitamin D-dependent route.
Calcium
Calcium is the most abundant mineral in the body. Approximately99%of total body calcium is found in the skeleton,with only small amounts in the plasma and extra-vascular?uid.Precise calcium requirements are uncertain.In the newborn infant the total body Ca con-tent is around28g with98%in bone.Based on body composition measurements,approximately1kg of cal-cium is deposited in the skeleton between birth and adult-hood.Daily accretion rates for boys and girls must average around150and200mg calcium/d,however,since growth is not uniform,accretion rates may be as high as 400mg calcium/d during infancy and puberty.A recent study using dual energy x-ray absorptiometry found an average bone calcium accretion rate of220mg/d and 317mg/d in girls and boys respectively during stage III puberty(66).The amount of dietary calcium needed to satisfy the demand for skeletal growth and mineralization is greater than the theoretical accretion rate because of incomplete calcium absorption and losses from skin,urine and gastrointestinal tract.The limited information avail-able regarding calcium needs in children is re?ected in wide variation in recommended intakes(22,67,68),and is generally based on recommended oral intake of calcium. Administration of intravenous calcium during parenteral nutrition is limited by solubility.
Phosphorus
Phosphorus(P)is a major intracellular mineral and also crucial for bone mineralisation.In newborn infants total body phosphorus is around16g(rising to600–900g in an adult)with80%in bone and9%in skeletal muscle. In the kidney85–90%of the?ltered phosphate is re-absorbed.In the presence of a low phosphate intake the kidney retains phosphate and it disappears from the
Recommendation
An intravenous selenium supply of2to3m g/kg
per day is recommended for parenterally fed
LBW infants.GOR D
Recommendations
Parenteral zinc supply is recommended in daily
dosages of450–500m g/kg per day for premature
infants,250m g/kg per day for infants less than3
months,100m g/kg per day for infants aged3
months or older,and50m g/kg per day(up to
a maximum of5.0mg/day)for children.GOR D
Excessive cutaneous or digestive losses of zinc
require additional supplementation.GOR D
GUIDELINES ON PAEDIATRIC PARENTERAL NUTRITION S43
J Pediatr Gastroenterol Nutr,Vol.41,Suppl.2,November2005
urine.Hypercalcaemia and hypercalciuria may result from phosphate de?ciency.Excess phosphate intake may lead to hyperphosphataemia,hypocalcaemia and second-ary hyperparathyroidism.De?ciency of phosphate results in bone demineralisation and rickets.Extreme hypo-phosphataemia can be precipitated by nutritional restitu-tion(?refeeding syndrome?)and can result in muscle paralysis,cardiac dysfunction and respiratory failure.
Magnesium
Magnesium is the fourth most abundant metal in the body and the second most abundant intracellular electrolyte.In the newborn infant the total body Mg is around0.8g(rising to25g in an adult)with60%in bone. The physiological importance of magnesium lies in its role in skeletal development and in the maintenance of electrical potential in nerves and muscle membranes. Calcium homoeostasis is controlled in part by a Mg requiring mechanism which releases parathyroid hormone.Plasma Mg represents only0.3to11%of total body stores and total plasma Mg concentration does not estimate the biologically active fraction-ionised Mg(69). Inadequate intakes of Mg,Ca and P may induce rickets, fractures,impaired bone mineralization and reduced linear growth(70,71).
Parenteral Supply of Ca and P
In selecting compounds suitable for parenteral nutri-tion it must be considered that Ca cations may precipitate with inorganic phosphate anions.To some degree this can be avoided by mixing Ca and phosphate with amino-acids and glucose(72–75)but even more so by using organic phosphorus compounds(76–85).Glycerophos-phate is available as di-sodium salt in Europe.Parenteral solutions containing Ca may cause damage to peripheral veins,and extravasation may induce severe tissue ne-crosis.The adequacy of Ca and P intakes in young infants should be adjusted until both are excreted simultaneously with low urine concentrations(1–2mmol/L)indicative of a slight surplus(86).
Calcium,Phosphate and Magnesium in Children Taking into account percentage absorption from the diet,parenteral intakes of Ca,P and Mg can be estimated from Recommended Nutrient Intakes(RNI),the amount of nutrient that is enough,or more than enough,for about 97%of people in the group(87).Around66%of calcium is absorbed from breast milk,but net dietary absorption in older children is around half this level.Absorption of phosphorus is about60%with the RNI for phosphorus being set equal to that for calcium in mmol(87).Between 20-50%of dietary magnesium is absorbed,but much more can be absorbed when dietary intakes are low. Recommendations for parenteral intake of Ca,P and Mg are given in the tables below.Blood concentrations re-quire periodic monitoring;phosphate concentration may drop suddenly in malnourished patients starting PN. Recommended parenteral calcium,phosphorus and magnesium intakes for infants and children are shown in Table7.1.GOR D
Calcium and Phosphorus in the
Premature Newborn
The total amounts of Ca and P accreted in foetal life are strongly correlated with body weight(88–91).This was con?rmed for the bone mineral content in newborn infants including those with intrauterine growth re-tardation(92).In preterm infants the retention of Ca and P is proportional to growth(93).Foetal bone mineral accretion rate can be achieved in preterm infants given suf?cient supplementation with Ca and P(86).
Requirements
The foetal mineral accretion rate corresponds to 2.0mmol Ca/10g newly grown body weight and 1.52mmol P respectively.This has been proposed as a reference mark for parenteral nutrition of infants born preterm and at term.The dosage should be adjusted to the individual growth per body weight.Preterm infants growing at a rate of20g/d need4.0mmol Ca and3.0P per infant and day to meet the foetal requirements.If the baby weighs1.0kg this dose would correspond to4and 3mmol/kg per day.If the baby weighs2kg then this dose would correspond to2and1.5mmol/kg per day.If the baby is growing at a slower rate(10g per day)the dose would correspond to only1mmol Ca and0.75mmol P/kg per day.Therefore,a wide range covers the spectrum of requirements:Ca 1.0–4.0mmol/kg per day,P0.75–3.0mmol/kg per day which provides a molar Ca:P ratio of1.3.(64,65).
TABLE7.1.Recommended parenteral Ca,P,and Mg intake Age
Suggested parenteral
intake Ca mg
(mmol)/kg
Suggested parenteral
intake P mg
(mmol)/kg
Parenteral
intake Mg mg
(mmol)/kg 0–6m32(0.8)14(0.5)5(0.2)
7–12m20(0.5)15(0.5) 4.2(0.2)
1–13y11(0.2)6(0.2) 2.4(0.1) 14–18y7(0.2)6(0.2) 2.4(0.1)
Recommendations
Growing newborn infants should usually receive
1.3–3mmol calcium/kg per day and1–
2.3mmol
phosphorus/kg per day,with a Ca:P ratio(mol/mol)
in the range of1.3–1.7.GOR D
S44GUIDELINES ON PAEDIATRIC PARENTERAL NUTRITION J Pediatr Gastroenterol Nutr,Vol.41,Suppl.2,November2005
REFERENCES
1.Ben Hariz M,Goulet O,De Potter S,et al.Iron overload in children
receiving prolonged parenteral nutrition.J Pediatr1993;123:238–41.
2.Patruta SI,Horl WH.Iron and infection.Kidney Int Suppl1999;69:
S125–30.
3.Ellison RT,Giehl TJ.Killing of gram-negative bacteria by
lactoferrin and lysozyme.J Clin Invest1991;88:1080–91.
4.Hershko CH.Iron and infection.In:Hallberg L,Asp GA,eds.Iron
Nutrition in Health and Disease.New York:John Libbey& Company;1996:231–8.
5.Fahmy M,Young SP.Modulation of iron metabolism in monocyte
cell line U937by in?ammatory cytokines:changes in transferrin uptake,iron handling and ferritin mRNA.Biochem J1993;296: 175–81.
6.Rudd MJ,Good MF,Chapman DE,et al.Clonal analysis of the
effect of iron on human cytotoxic and proliferating T lymphocytes.
Immunol Cell Biol1990;68:317–24.
7.Chandra RK,Saraya AK.Impaired immunocompetence associated
with iron de?ciency.J Pediatr1975;86:899–902.
8.Reddy S,Adcock KJ,Adeshina H,et al.Immunity,transferrin,and
survival in kwashiorkor.Br Med J1970;4:268–70.
9.Melby K,Slordahl S,Gutteberg TJ,et al.Septicaemia due to
Yersinia enterocolitica after oral overdoses of iron.Br Med J(Clin Res Ed)1982;285:467–8.
10.Ball PA.Iron in pediatric parenteral nutrition:are we getting rusty?
Nutrition1999;15:815–6.
11.Burns DL,Pomposelli JJ.Toxicity of parenteral iron dextran
therapy.Kidney Int Suppl1999;69:119S–124.
12.Khaodhiar L,Keane-Ellison M,Tawa NE,et al.Iron de?ciency
anemia in patients receiving home total parenteral nutrition.JPEN J Parenter Enteral Nutr2002;26:114–9.
13.Reed MD,Bertino JS,Halpin https://www.doczj.com/doc/c24302467.html,e of intravenous iron dextran
injection in children receiving total parenteral nutrition.Am J Dis Child1981;135:829–31.
14.Hamstra RD,Block MH,Schock,et al.Intravenous iron dextran in
clinical medicine.JAMA1980;243:1726–31.
15.James BE,Hendry PG,MacMahon RA.Total parenteral nutrition of
premature infants.2.Requirement for micronutrient elements.Aust Paediatr J1979;15:67–71.
16.Friel JK,Andrews WL,Hall MS,et al.Intravenous iron
administration to very-low-birth-weight newborns receiving total and partial parenteral nutrition.JPEN J Parenter Enteral Nutr1995;
19:114–8.
17.Van der Zee J,Krootjes BB,Chignell CF,et al.Hydroxyl radical
generation by a light-dependent Fenton reaction.Free Radic Biol Med1993;14:105–13.
https://www.doczj.com/doc/c24302467.html,voie JC,Chessex P.Bound iron admixture prevents the
spontaneous generation of peroxides in total parenteral nutrition solutions.J Pediatr Gastroenterol Nutr1997;25:307–11.
19.Vaughan LM,Small C,Plunkett V.Incompatibility of iron dextran
and a total nutrient admixture.Am J Hosp Pharm1990;47: 1745–6.
20.Allwood MC,Kearney https://www.doczj.com/doc/c24302467.html,patibility and stability of additives
in parenteral nutrition admixtures.Nutrition1998;14:697–706. 21.Barry DM,Reeve AW.Increased incidence of gram-negative
neonatal sepsis with intramuscula iron administration.Pediatrics 1977;60:908–12.
22.Greene HL,Hambidge KM,Schanler R,et al.Guidelines for the
use of vitamins,trace elements,calcium,magnesium,and phosphorus in infants and children receiving total parenteral nutrition:report of the Subcommittee on Pediatric Parenteral Nutrient Requirements from the Committee on Clinical Practice Issues of the American Society for Clin Nutr.Am J Clin Nutr1988;
48:1324–42.
23.Shulman RJ.New developments in total parenteral nutrition for
children.Curr Gastroenterol Rep2000;2:253–8.
24.Van Gossum A,Neve J.Trace element de?ciency and toxicity.Curr
Opin Clin Nutr Metab Care1998;1:499–507.25.Schanler RJ,Shulman RJ,Prestridge LL.Parenteral nutrient needs
of very low birth weight infants.J Pediatr1994;125:961–8.
https://www.doczj.com/doc/c24302467.html,mittee on Nutrition.American Academy of Pediatrics.
Nutritional needs of preterm infants.In:Kleinman RE,ed.Pediatric nutrition handbook.Elk Grove Village:American Academy of Pediatrics;1998:55–88.
27.Papageorgiou T,Zacharoulis D,Xenos D,et al.Determination of
trace elements(Cu,Zn,Mn,Pb)and magnesium by atomical absorption in patients receiving total parenteral nutrition.Nutrition 2002;18:32–4.
28.Yu VY.Principles and practice of parenteral nutrition in the
neonatal period.Acta Med Port1997;10:185–96.
29.Leung FY,Galbraith LV.Elevated serum chromium in patients on
total parenteral nutrition and the ionic species of contaminant chromium.Biol Trace Elem Res1995;50:221–8.
30.Lovrincevic I,Leung FY,Al?eri MA,et al.Can elevated chromium
induce somatopsychic responses?Biol Trace Elem Res1996;55: 163–71.
31.Bougle D,Bureau F,Deschrevel G,et al.Chromium and par-
enteral nutrition in children.J Pediatr Gastroenterol Nutr1993;
17:72–4.
32.Moukarzel AA,Song MK,Buchman AL,et al.Excessive
chromium intake in children receiving total parenteral nutrition.
Lancet1992;339:385–8.
33.Hak EB,Storm MC,Helms RA.Chromium and zinc contamination
of parenteral nutrient solution components commonly used in infants and children.Am J Health Syst Pharm1998;55:150–4. 34.Araya M,Olivares M,Pizarro F,et al.Copper exposure and potential
biomarkers of copper metabolism.Biometals2003;16:199–204. 35.Cordano A.Clinical manifestations of nutritional copper de?ciency
in infants and children.Am J Clin Nutr1998;67:1012S-6S.
36.Cunningham JJ,Leffell M,Harmatz P.Burn severity,copper dose,
and plasma ceruloplasmin in burned children during total parenteral nutrition.Nutrition1993;9:329–32.
37.Barclay SM,Aggett PJ,Lloyd DJ,et al.Reduced erythrocyte
superoxide dismutase activity in low birth weight infants given iron supplements.Pediatr Res1991;29:297–301.
38.Fell JM,Reynolds AP,Meadows N,et al.Manganese toxicity in
children receiving long-term parenteral https://www.doczj.com/doc/c24302467.html,ncet1996;347: 1218–21.
39.Cunningham JJ,Lydon MK,Briggs SE,et al.Zinc and copper status of
severely burned children during TPN.J Am Coll Nutr1991;10:57–62.
40.Moukarzel AA,Buchman AL,Salas JS,et al.Iodine supplemen-
tation in children receiving long-term parenteral nutrition.J Pediatr 1992;121:252–4.
41.Reynolds AP,Kiely E,Meadows N.Manganese in long term
paediatric parenteral nutrition.Arch Dis Child1994;71:527–8. 42.Kelly DA.Liver complications of pediatric parenteral nutrition-
epidemiology.Nutrition1998;14:153–7.
43.Fok TF,Chui KK,Cheung R,et al.Manganese intake and
cholestatic jaundice in neonates receiving parenteral nutrition:
a randomized controlled study.Acta Pediatr2001;90:1009–15.
44.Masumoto K,Suita S,Taguchi T,et al.Manganese intoxication
during intermittent parenteral nutrition:report of two cases.JPEN J Parenter Enteral Nutr2001;25:95–9.
45.Puntis JW.Nutritional support at home and in the community.Arch
Dis Child2001;84:295–8.
46.Ono J,Harada K,Kodaka R,et al.Manganese deposition in the
brain during long-term total parenteral nutrition.JPEN J Parenter Enteral Nutr1995;19:310–2.
47.Kafritsa Y,Fell J,Long S,et al.Long-term outcome of brain
manganese deposition in patients on home parenteral nutrition.
Arch Dis Child1998;79:263–5.
48.Komaki H,Maisawa S,Sugai K,et al.Tremor and seizures as-
sociated with chronic manganese intoxication.Brain Dev1999;21: 122–4.
49.Friel JK,MacDonald AC,Mercer CN,et al.Molybdenum
requirements in low-birth-weight infants receiving parenteral and enteral nutrition.JPEN J Parenter Enteral Nutr1999;23:155–9.
GUIDELINES ON PAEDIATRIC PARENTERAL NUTRITION S45
J Pediatr Gastroenterol Nutr,Vol.41,Suppl.2,November2005
50.Inder TE,Darlow BA,Sluis KB,et al.The correlation of elevated
levels of an index of lipid peroxidation(MDA-TBA)with adverse outcome in the very low birthweight infant.Acta Paediatr1996;85: 1116–22.
51.Kretzer FL,Hittner HM.Retinopathy of prematurity:clinical im-
plications of retinal development.Arch Dis Child1988;63:1151–67.
52.Litov RE,Combs GF.Selenium in pediatric nutrition.Pediatrics
1991;87:339–51.
53.Terada A,Nakada M,Nakada K,et al.Selenium administration to
a ten-year-old patient receiving long-term total parenteral nutrition
(TPN)-changes in selenium concentration in the blood and hair.
J Trace Elem Med Biol1996;10:1–5.
54.Sando K,Hoki M,Nezu R,et al.Platelet glutathione peroxidase
activity in long-term total parenteral nutrition with and without selenium supplementation.JPEN J Parenter Enteral Nutr1992;16: 54–8.
55.Daniels L,Gibson R,Simmer K.Selenium status of preterm infants:
the effect of postnatal age and method of feeding.Acta Paediatr 1997;86:281–8.
56.Klinger G,Shamir R,Singer P,et al.Parenteral selenium
supplementation in extremely low birth weight infants:inadequate dosage but no correlation with hypothyroidism.J Perinatol1999;
19:568–72.
57.Kelly DA,Coe AW,Shenkin A,et al.Symptomatic selenium de-
?ciency in a child on home parenteral nutrition.J Pediatr Gastro-enterol Nutr1988;7:783–6.
58.Daniels L,Gibson R,Simmer K.Randomised clinical trial of
parenteral selenium supplementation in preterm infants.Arch Dis Child Fetal Neonatal Ed1996;74:F158–64.
59.Huston RK,Jelen BJ,Vidgoff J.Selenium supplementation in
low-birthweight premature infants:relationship to trace metals and antioxidant enzymes.JPEN J Parenter Enteral Nutr1991;15: 556–9.
60.Makhoul IR,Sammour RN,Diamond E,et al.Selenium concen-
trations in maternal and umbilical cord blood at24–42weeks of gestation:basis for optimization of selenium supplementation to premature infants.Clin Nutr2004;23:373–81.
61.Zlotkin SH,Buchanan BE.Amino acid intake and urinary zinc
excretion in newborn infants receiving total parenteral nutrition.Am J Clin Nutr1988;48:330–4.
62.Friel JK,Andrews WL.Zinc requirement of premature infants.
Nutrition1994;10:63–5.
63.Leung FY.Trace elements in parenteral micronutrition.Clin
Biochem1995;28:561–6.
64.Leitch I.The determination of the calcium requirements of man.
Nutr Abstr Rev Ser Hum Exp1937;6:553–78.
65.Leitch I,Aitken FC.The estimation of calcium requirement:a re-
examination.Nutr Abstr Rev Ser Hum Exp1959;29:393–411. 66.Molgaard C,Thomsen BL,Michaelsen KF.Whole body bone
mineral accretion in healthy children and adolescents.Arch Dis Child1999;81:10–5.
67.Evans TJ,Cockburn F.Parenteral feeding.In:McLaren DS,
Burman D,Belton NR,et al.Textbook of Paediatric Nutrition.
Edinburgh:Churchill Livingstone;1991:342.
68.Heird WC.Total parenteral nutition.In:Lebenthal E,ed.Textbook
of gastroenterology and nutrition in infancy.New York:Raven Press;1981:663.
69.Maggioni A,Orzalesi M,Mimouni FB.Intravenous correction of
neonatal hypomagnesemia:effect on ionized magnesium.J Pediatr 1998;132:652–5.
70.Giles MM,Laing IA,Elton RA,et al.Magnesium metabolism
in preterm infants:effects of calcium,magnesium,and phospho-rus,and of postnatal and gestational age.J Pediatr1990;117: 147–54.
71.Koo WW,Tsang RC.Mineral requirements of low-birth-weight
infants.J Am Coll Nutr1991;10:474–86.
72.Dunham B,Marcuard S,Khazanie PG,et al.The solubility of
calcium and phosphorus in neonatal total parenteral nutrition solutions.JPEN J Parenter Enteral Nutr1991;15:608–11.73.Fitzgerald KA,MacKay MW.Calcium and phosphate solubility in
neonatal parenteral nutrient solutions containing TrophAmine.Am J Hosp Pharm1986;43:88–93.
74.Poole RL,Rupp CA,Kerner JA.Calcium and phosphorus in
neonatal parenteral nutrition solutions.JPEN J Parenter Enteral Nutr1983;7:358–60.
75.Venkataraman PS,Brissie EO,Tsang RC.Stability of calcium and
phosphorus in neonatal parenteral nutrition solutions.J Pediatr Gastroenterol Nutr1983;2:640–3.
76.B€a ssler KH,Hassinger W.Die Eignung von DL-Glyzerin-3-
phosphat zur parenteralen Substitution von anorganischem Phos-phat.Infusionstherapie1976;3:138–42.
77.Colonna F,Candusso M,de V onderweid U,et al.Calcium and
phosphorus balance in very low birth weight babies on total parenteral nutrition.Clin Nutr1990;9:89–95.
78.Costello I,Powell C,Williams AF.Sodium glycerophosphate in the
treatment of neonatal hypophosphataemia.Arch Dis Child Fetal Neonatal Ed1995;73:44F–45.
79.Devlieger H,Meyers Y,Willems L,et al.Calcium and
phosphorus retention in the preterm infant during total parenteral nutrition.A comparative randomised study between organic and inorganic phosphate as a source of phosphorus.Clin Nutr1993;
12:277–81.
80.Draper HH,Yuen DE,Whyte RK.Calcium glycerophosphate as
a source of calcium and phosphorus in total parenteral nutrition
solutions.JPEN J Parenter Enteral Nutr1991;15:176–80.
81.Hanning RM,Atkinson SA,Whyte RK.Ef?cacy of calcium
glycerophosphate vs conventional mineral salts for total parenteral nutrition in low-birth-weight infants:a randomized clinical trial.
Am J Clin Nutr1991;54:903–8.
82.Hanning RM,Mitchell MK,Atkinson SA.In vitro solubility of
calcium glycerophosphate versus conventional mineral salts in pediatric parenteral nutrition solutions.J Pediatr Gastroenterol Nutr1989;9:67–72.
83.Prinzivalli M,Ceccarelli S.Sodium d-fructose-1,6-diphosphate
vs.sodium monohydrogen phosphate in total parenteral nutri-tion:a comparative in vitro assessment of calcium phos-phate compatibility.JPEN J Parenter Enteral Nutr1999;23: 326–32.
84.Raupp P,von Kries R,Pfahl HG,et al.Glycero-vs glucose-
phosphate in parenteral nutrition of premature infants:a compara-tive in vitro evaluation of calcium/phosphorus compatibility.JPEN J Parenter Enteral Nutr1991;15:469–73.
85.Ronchera-Oms CL,Jime′nez NV,Peidro J.Stability of parenteral
nutrition admixtures containing organic phosphates.Clin Nutr 1995;14:373–80.
86.Pohlandt F.Prevention of postnatal bone demineralization in
very low-birth-weight infants by individually monitored supple-mentation with calcium and phosphorus.Pediatr Res1994;35: 125–9.
87.Department of Health.Report on Health and Social Services41.
Dietary reference values for food and energy and nutrients for the United Kingdom.London:HMSO;1991.
88.Fee BA,Weil WB.Body composition of infants of diabetic mothers
by direct analysis.Ann N Y Acad Sci1963;110:869–97.
89.Kelly HJ,Sloan RE,Hoffman W,et al.Accumulation of nitrogen
and six minerals in the human fetus during gestation.Hum Biol 1951;23:61–74.
90.Widdowson EM,Spray CM.Chemical development in utero.Arch
Dis Child1951;26:205–14.
91.Widdowson EM,Dickerson JWT.The composition of the body as
a whole.In:Comar CL,Bronne F,eds.Mineral Metabolism.New
York:Academic Press;1961:V ol.II Pt.A.
92.Pohlandt F,Mathers N.Bone mineral content of appropriate and
light for gestational age preterm and term newborn infants.Acta Paediatr Scand1989;78:835–9.
93.Trotter A,Pohlandt F.Calcium and phosphorus retention in ex-
tremely preterm infants supplemented individually.Acta Paediatr 2002;91:680–3.
S46GUIDELINES ON PAEDIATRIC PARENTERAL NUTRITION J Pediatr Gastroenterol Nutr,Vol.41,Suppl.2,November2005
肠外肠内营养临床指南(2006 版)(草案) 第一部分总论 第二部分成人营养需要量 第三部分营养风险筛查(NRS) 第四部分肠外营养素 第五部分输注路径 第六部分疾病营养支持 一.术后糖电解质输液 二.围手术期肠外营养 三.围手术期肠内营养 四.危重病 五.成人烧伤 六.胰腺炎 七.短肠综合征与胃肠道瘘 八.炎性肠病 九.肝脏疾病与肝移植 十.心血管疾病 十一.神经性疾病 十二.糖尿病 Ⅱ.肠外肠内营养临床指南(2006 版)(草案) 第一部分总论 中华医学会肠外肠内营养学分会(Chinese Society of Parenteral and Enteral Nutrition, CSPEN)于2004年12月在京成立。作为一个多学科学术组织,CSPEN的愿景(vision)是倡导循证营养实践,促进我国肠外肠内营养的合理应用,为患者提供安全、有效和具有良好效价比的营养治疗。编写、制定与推广临床指南是实现上述目标的重要途径。指南定义为:按照循证医学原则,以当前最佳证据为依据,按照系统和规范方法,在多学科专家、大中规模医院的临床医师和护理人员合作下达成的共识。 本指南的宗旨是为临床医师、护理工作者、营养师和患者在特定临床条件下,制定和/或接受肠外肠内营养治疗方案提供帮助,并为卫生政策的制定者提供决策依据。 2005年,CSPEN组织我国临床营养、儿科、外科、内科等多学科专家成立了第一届《肠外肠内营养指南》编写委员会,于当年制定和公布了第一版《肠外肠内营养学临床―指南‖系列一:住院患者肠外营养支持的适应证》,先后在《中国临床营养杂志》、《中华医学杂志》和《中华外科杂志》登载。这是我国首个按照循证医学原则制定的肠外肠内营养指南,出版后受到国内同行的关注。 2006年版指南制订过程 在2005年版的基础上,2006年1月,CSPEN开始组织《肠外和肠内营养临床指南》修订工作。在广泛听取和收集国内同行意见和建议的基础上,2006年4月,召开了2006版指南第一次“共识工作会议”,讨论重
肠道外营养疗法的指南
肠道外营养疗法的指南 一、适应证 (一)肠功能障碍:如短肠综合征、严重小肠疾病、放射性肠炎、严重腹泻及顽固性呕吐胃肠梗阻、肠外瘘等; (二)重症胰腺炎; (三)高代谢状态危重患者:如大手术围手术期、大面积烧伤、多发性创伤等; (四)严重营养不足肿瘤患者; (五)重要器官功能不全患者:如肝、肾、肺、心功能不全或衰竭等; (六)大剂量化疗、放疗或接受骨髓移植患者。 二、禁忌证 (一)胃肠功能正常,能获得足量营养者; (二)需急诊手术者,术前不宜强求肠外营养; (三)临终或不可逆昏迷患者。 三、并发症 (一)导管相关并发症 1、机械性并发症:均与放置中心静脉导管有关。常见的有气胸、血胸、动脉损伤、神经损伤、胸导管损伤、空气或导管栓塞、静脉血栓形成等。发生后需拔除导管,治疗并发症,从其他静脉另行
降低血渗透压,同时正规胰岛素以1O~20U/h经静脉滴入。在纠正过程中要防止血糖下降太快而导致脑细胞水肿。 2)低血糖:突然中止PN液的输入,而血胰岛素仍处于较高水平,就极易发生低血糖,故 PN 液输入突然中止应视为禁忌。不应利用同一静脉途径输血或输注其他不含糖类液体而停止 PN 。对有糖代谢异常者,可用等渗葡萄糖液500ml作为过渡,然后完全停用PN 。 2、氨基酸代谢紊乱: 以水解蛋白为主要氮源时,易发生高血氨症或氮质血症。目前普遍使用结晶氨基酸液作为氮源,已很少发生; 3、脂肪代谢紊乱: 接受PN治疗3~6周以上,若PN液中不含脂肪,则可能发生必需脂肪酸缺乏症。预防的最好方法是每天补充脂肪乳剂,每周至少输注脂肪乳剂2次; 4、电解质及微量元素缺乏: 实施PN时,电解质需要量增加,不注意及时补充时极易发生电解质缺乏症,低钾、低磷、低钙和低镁血症均可出现。微量元素最常见的是锌缺乏,其次为铜缺乏和铬缺乏。凡是长期行PN治疗者,应每天补充微量元素。 (三)肝胆系统并发症 PN 时易引起胆汁淤积性肝功能不全,其原因很多,其中长期能量过高、肠内长期没有含脂肪食物通过是重要原因。可通过调整营养液用量和配方使其纠正。
肠外肠临床营养指南手册 医学院附属医院营养科二O一一年六月
20世纪60年代末,肠外营养(PN)与肠营养(EN)相继应用于临床,取得了明显的效果,使许多病人得到康复,同时临床营养的输液技术和疾病代有了广泛、深入的研究。40年来,在营养制剂、输液方法和代理论上,都有着迅速的发展、进步,甚至有些概念也在改变。如在开始阶段提出要给予高热量,应用了Hyperalimenlation一词,经临床实践证明,给予超高热量并不能被机体所接受。在机体应激状况下,即使是根据测定或计算的热量都难以给予,并且还有加重机体代紊乱的可能,从而提出了低热量(hypocaloric)的概念。其后又发现,长期低热量营养有损于机体的恢复,在应用上要有一定的时限性。社会的发展是在实践中反复改善而进步的。医学亦然,在实践中不断认识,不断提高。临床营养支持是一门新兴技术,人们对它的认识更是频繁的在更改,逐步深入,不断发展。 本指南由中华医学会肠外肠营养学分会(Chinese Society of Parenteral and Enteral Nutrition, CSPEN)制订并发布,是临床营养学的重要参考资料,可以指导临床医生包括临床营养医生制订规化的序贯肠肠外营养治疗方案,对提高临床营养支持的安全性和功效具有很强的指导意义。 如有不明之处,请与营养科联系。 二O一一年六月
常用名词定义 (5) 第一章成人营养素需要量 (6) 一、背景 (6) 二、证据 (6) 三、推荐意见 (7) 第二章住院患者营养风险筛查 (9) 一、背景 (9) 二、证据 (9) 三、推荐意见 (10) 第三章肠外营养素 (11) 第一节氨基酸 (11) 一、背景 (11) 二、证据 (11) 三、推荐意见 (11) 第二节脂肪乳 (11) 一、背景 (11) 二、证据 (12) 三、推荐意见 (13) 第四章营养支持输注系统 (13) 第一节肠营养管饲途径 (13) 一、背景 (13) 二、证据 (14) 三、推荐意见 (14) 第二节肠营养输注泵 (Enteral Feeding Pump) (14) 一、背景 (14) 二、证据 (15) 三、推荐意见 (15) 第三节肠外营养输注途径 (15) 一、背景 (15) 二、证据 (16) 三、推荐意见 (17) 第五章疾病营养支持 (19) 第一节术后糖电解质输液 (19) 一、背景 (19) 二、证据 (19) 三、推荐意见 (20) 第二节围手术期肠外营养 (21) 一、背景 (21) 二、证据 (21) 三、推荐意见 (22) 第三节围手术期肠营养 (22) 一、背景 (22) 二、证据 (22) 三、推荐意见 (23)
【最新整理,下载后即可编辑】 **市人民医院 肠外营养药物使用指南 全肠外营养(TPN)药物是经静脉途径供应患者所需的营养要素,包括热量(碳水化合物、脂肪乳)、必需和非必需氨基酸、维生素、电解质及微量元素,以抑制分解代谢、促进合成代谢,并维持细胞、器官结构与功能的需要。 营养支持的适应症、肠外营养剂的选择、营养液的配制及输注方法、途径、护理都会影响患者的恢复治疗,因此,规范化的营养支持模式势在必行,从而避免在营养支持过程中发生不合理现象,最大程度保证为患者提供安全、合理、有效、经济的营养支持。 一、肠外营养的适应证 (一)重度营养风险或蛋白质-能量营养不良,经口或经肠道营养素摄入不足,且短期内(10~14天)无法恢复正常进食者。 (二)胃肠功能障碍。 (三)胃肠道梗阻、消化道瘘、短肠综合征。 (四)重症活动期炎症性肠病,无法耐受肠内营养支持。 (五)重症胰腺炎,肠内营养出现不良反应或热量供应不足时,须联合应用肠外营养。 (六)重症胰腺炎,无法耐受肠内营养时。 (七)放射性肠炎。 二、肠外营养的禁忌证 (一)严重水、电解质紊乱,酸碱平衡失调。 (二)休克、器官功能衰竭终末期。 (三)下列情况慎用肠外营养: 1、无明确治疗目的或已确定为不可治愈而盲目延长治疗者:如广泛转移的晚期恶性肿瘤伴恶病质的患者,生活质量差、任何治疗方法均无明显改善作用,此时肠外营养也无明显益处,反而会增加患者生理和经济负担。 2、胃肠道功能正常或有肠内营养适应证者:对接受肠外营养支持的患者,应注意观察胃肠道功能恢复情况,及时有肠外营养过渡到肠内营
养。 3、患者一般情况良好,预计需要肠外营养少于5天者。 4、原发病需立即进行急诊手术者。 5、预计发生肠外营养并发症的危险性大于其可能带来的益处者。 6、心血管功能紊乱或严重代谢紊乱尚未控制或处于纠正期间。 7、脑死亡或临终或不可逆昏迷。 三、TPN合理配方设计原则 (一)静脉营养支持的模式是个体化给药,在配方上应突出个体化的特点。 (二)TPN的配方没有统一的处方,处方设计应全面考虑,包括是否有使用TPN的指证、患者的年龄、性别、体重或体表面积及病情。 (三)合理处方设计应全面了解患者的营养状况、水、电解质及酸碱平衡情况、肝肾功能等。 (四)处方设计患者所需的总热量、液体量、糖、脂肪、氨基酸、电解质、微量元素等的用量和比值,应尽量达到合理的个体化配方。 (五)处方设计还应考虑各营养成分的理化性质、配伍禁忌及影响TPN稳定性的因素。 四、营养风险筛查评估工具 (一)主观全面评价方法(SGA)★(附件一) (二)住院患者营养风险筛查NRS-2002评估表★(附件二) 五、计算所需热量 (一)根据Harris Bennedict(BEE)公式计算: 男性:BEE(kcal/24h)=66.5+13.8W+5.0H-6.8A 女性:BEE(kcal/24h)=655+9.5W+1.8H-4.7A W-体重(kg)H-身高(cm)A-年龄(岁)1kcal=4.184kJ 低度应激=1.3×BEE 严重应激=2.0×BEE 中度应激=1.5×BEE 恶性肿瘤=1.6×BEE 注:应激状态是指机体在饥饿,创伤,感染后和疾病时的代谢变化反应,交感神经引起的高代谢状态,使机体的静息能量消耗(REE)增加。能量消耗增加幅度比想象低,创伤、感染时视其严重程度REE可增加20%~30%,只有大面积烧伤的REE才会增加50%~100%,通常的择期手术,REE仅增加约10%左右。
ICU肠外肠内营养支持指南流程图(EN)1表: CSPEN-ICU 禁忌证: 难以耐受经口EN 到ICU <24小时 需进一步监测、评估 禁忌证:急性胰腺炎 肠管吻合术后 肠管缺血损伤肠痿 急诊肠切除术急诊内窥镜 术肠梗阻 高位鼻胃功能损伤炎性肠 病加重 *仍然需要营养支持 开始TPN: 应用加入谷氨酰胺的TPN 每12小时评估EN指证 开始TPN适应证:应用加 入谷氨酰胺的TPN 每12小时 评估EN指证增至100% 达到目标?
ICU肠外肠内营养支持指南流程图(EN)1表: CSPEN-ICU 病人能经口进食吗?是 ----- ?经口进食(能摄入80%以上的营养)「否 胃肠是否'有功能?----------------------- ? 肠外营养有11是预消化配方 消化吸收功能? ---------------- ? r否是 肠道功能问题? (腹泻便秘)疋 ---- ? 膳食纤维配方 肠外肠内营养支持ICU—营养制剂的选 择 标准配方
ICU肠外肠内营养支持指南流程图(EN)1表: CSPEN-ICU 患者腹泻? 大便形态具有临床阳性体征? 临床应用药物 适应证? 患者临床应用 敏感抗生素? 持续EN 否?原医嘱执行 疋调整药物及营养素 ■适应EN 是 选择不同营养素 ■辅助EN EN患者禁忌证: 1腹泻临床阳性体征 1水样便〉300ml每天 2)大便失禁〉4次每天 3)导管或创口污染风险 2、EN后明显腹胀、反流 3、增加腹部并发症风险 4、临床需要胃肠负压吸引 5、胃潴留〉200ml EN后 选择 要素营养素? 腹泻好转? 是 . 恢复EN 原医嘱执行 药物引起腹泻原因: 灭吐灵; 氨茶碱;镁剂; 红霉素; 木糖醇; 磷制剂; 奎尼丁; 甘露醇; 减少量或次数直到好转 恢复EN 原医嘱执行
肠道外营养疗法的指南 一、适应证 (一)肠功能障碍:如短肠综合征、严重小肠疾病、放射性肠炎、严重腹泻及顽固性呕吐胃肠梗阻、肠外瘘等; (二)重症胰腺炎; (三)高代谢状态危重患者:如大手术围手术期、大面积烧伤、多发性创伤等; (四)严重营养不足肿瘤患者; (五)重要器官功能不全患者:如肝、肾、肺、心功能不全或衰竭等; (六)大剂量化疗、放疗或接受骨髓移植患者。 二、禁忌证 (一)胃肠功能正常,能获得足量营养者; (二)需急诊手术者,术前不宜强求肠外营养; (三)临终或不可逆昏迷患者。 三、并发症 (一)导管相关并发症 1、机械性并发症:均与放臵中心静脉导管有关。常见的有气胸、血胸、动脉损伤、神经损伤、胸导管损伤、空气或导管栓塞、静脉血栓形成等。发生后需拔除导管,治疗并发症,从其他静脉另行臵管。
2、感染性并发症:主要是导管性败血症,是PN时最常见、最严重的并发症。可因穿刺时未严格执行无菌技术、导管护理不当、营养液细菌污染、导管放臵时间过长或患者存有感染病灶引起。发生后应立即拔除导管,作血培养和导管头培养,改用周围静脉营养。若血培养阳性,则应根据药敏试验选用抗生素。预防的措施为严格执行无菌穿刺插管技术、穿刺导管经 15cm 的皮下隧道引出皮肤、在超净台内配制营养液、使用 3L 袋以组成全封闭式输液系统、保持导管出口处皮肤干燥、定时每天消毒穿刺导管周围皮肤、避免导管采血或输血、注意更换输液系统时的无菌操作等。 3、中心静脉导管拔除意外综合征:该并发症主要累及心、肺及中枢神经系统,出现难以解释的严重临床症状。预防的措施有在拔管前注意使患者取仰卧位或垂头仰卧位,当患者有脱水症时应避免拔管,导管拔出时嘱患者屏住呼吸,同时注意夹闭导管腔或用手指压在拔管的皮肤切口上,但要避免过度按压或用力摩擦颈动脉,切口处涂抗生素软膏,并嘱患者静卧 30 分钟。 (二)代谢性并发症 1、糖代谢紊乱: 1)高血糖和高渗性昏迷:因快速大量输入葡萄糖所致。预防措施是在输注 4h 后密切监测血糖水平。如发生高渗性昏迷,应立即停止葡萄糖输入,用低渗盐水(O.45)以950ml/h 的速度输入以降低血渗透压,同时正规胰岛素以1O~20U/h经静脉滴入。在纠正过程中要防止血糖下降太快而导致脑细胞水肿。
附录1 肠外肠内营养学临床指南 中华医学会肠外肠内营养学分会(2006 版) 第一章制定指南的“指南” 引言 制定指南的初级阶段 中华医学会肠外肠内营养学分会(Chinese Society of Parenteral and Enteral Nutrition, CSPEN)于2004年12月在京成立。作为一个多学科学术组织,CSPEN的愿景(vision)是倡导循证营养支持的实践,促进我国肠外肠内营养的合理应用,为患者提供安全、有效和具有良好效价比的营养治疗。 编写、制定与推广临床指南是实现上述目标的重要途径。指南定义为:按照循证医学原则,以当前最佳证据为依据,按照系统和规范方法,在多学科专家、各级医院的临床医师和护理人员合作下达成的共识。 本指南的宗旨是为临床医师、护理工作者、营养师、药剂师和患者在特定临床条件下,制定和/或接受肠外肠内营养支持方案提供帮助,并为卫生政策的制定者提供决策依据。 2005年1月- 9月,是我们分会制定指南的初级阶段。 CSPEN常委们在中华医学会的直接指导下,组织了我国肠外肠内营养学工作者及儿科、外科、内科等多学科专家成立了第一届《肠外肠内营养指南》编写委员会。按照循证医学原则,经过参比国内国外的临床研究报告,制定的肠外肠内营养支持的适应症指南。 在2005年9月在北京召开的的“第一届全国临床营养周”大会上公开征求意见后,又做了大范围的修正和大范围的补充,于当年12月完成了第2005版《肠外肠内营养学临床―指南‖系列一:住院患者肠外营养支持的适应证》。 虽然该指南范围窄,仅是住院患者肠外肠内营养支持的适应证的内容,但仍然受到业者的重视。已经先后在《中国临床营养杂志》、《中华医学杂志》和《中华外科杂志》等三本核心期刊杂志登载。发表后受到国内同行的关注,也为2006年完善方法学和扩大内容打下了基础。 一、2006年版指南制订过程
肠内营养治疗指南 营养是治疗疾病和健康长寿的保证。对患者来说,合理、平衡、及时的临床营养治疗极为重要。营养治疗包括肠内营养(enteral nutrition,EN)治疗和肠外营养(parenteral nutrition,PN)治疗,而前者又分为饮食治疗和管喂营养治疗。危重病人的营养治疗非常重要,俗话说“疾病三分治,七分养”,营养即在其中。任何时候都应遵循,如果胃肠存在,就应首先考虑使用肠内营养。与肠外相比,肠内营养经济、安全、方便,符合生理过程。 肠内营养制剂按蛋白来源分为两大类:一类是氨基酸型和短肽型(要素型)制剂(冬泽力);另一类是整蛋白型(非要素型)制剂(冬泽全)。每一类型的制剂中又可分为平衡型和疾病特异型。肠内营养制剂在国外还包括组件式肠内营养制剂。 为提高临床营养治疗效果,规范临床营养治疗程序,在参照国内外相关资料的基础上,结合冬泽特医专家的经验,制订营养治疗指南,供临床应用参考。 一、适应证 1、意识障碍、昏迷和某些神经系统疾病:如脑外伤、脑血管疾病、脑肿瘤、脑炎等所致的昏迷患者,老年痴呆不能经口进食或精神失常、严重抑郁症、神经性厌食者等。 2、吞咽困难和失去咀嚼能力:如咽下困难、口咽部外伤及手术后、重症肌无力者等。 3、上消化管梗阻或手术:如食管炎症、化学性损伤等造成咀嚼困难或吞咽困难、食管狭窄梗阻、食管癌、幽门梗阻、吻合口水肿狭窄、胃瘫等。 4、高代谢状态:如严重创伤、大面积烧伤、严重感染等所致机体高代谢、负氮平衡者。 5、消化管瘘:通常适用于低流量瘘或瘘的后期,如食管瘘、胃瘘、肠瘘、胆瘘、胰瘘等。对低位小肠瘘、结肠瘘及空肠喂养的胃十二指肠瘘效果最好。 6、术前准备和术后营养不良:如术前肠管准备期间、术中有额外营养素丢失者等。 7、炎性肠管疾病:如溃疡性结肠炎、Crohns病等。
XX医院 临床肠内及肠外营养操作指南第一节肠内营养 【肠内营养适应证及其优点】 1.口服摄入不足,但胃肠道有消化吸收功能的病人,可以应用肠内营养支持。 2.要努力实施肠内营养支持,即使暂时不成功也要尽可能创造条件去反复尝试肠内营养,因为临床病人一旦耐受了肠内营养,将受益无穷。 3.营养物质经门静脉系统吸收输送至肝脏,有利于内脏(尤其是肝脏)的蛋白质合成及代谢调节。 4.长期持续应用全肠外营养会使小肠粘膜细胞和营养酶系的活性退化,而肠内营养可以改善和维持肠道粘膜细胞结构与功能的完整性,有防止肠道细菌易位的作用。 5.肠外营养导致内脏血流与心搏出量增加,使代谢营养物质消耗的能量增加。 6.在同样热卡与氮量的条件下,应用肠内营养的病人的体重增长、氮潴留均优于全肠外营养,而且人体组成的改善也较明显。 7.肠内营养较价廉,对技术和设备的要求较低,使用简单,易于临床管理。 【肠内营养配方的选择】 1.可供临床选用的肠内营养配方很多,成分与营养价
值差别很大,选择配方时主要考虑其蛋白质、碳水化合物与脂肪的来源及比例,各配方的膳食纤维、维生素和矿物质含量也可能不同。肠内营养制剂发展迅速,配方常有改变,因此要注意所用产品的具体配方。 2.根据病人的营养状态及代谢状况确定营养需要量,高代谢病人应选择高热卡配方,需要限制水分摄入的病人应选择浓度较高的配方(如能量密度为1.5kcal/m1),免疫功能异常的病人应选择具有免疫调节作用的配方。 3.肠内营养支持提供的非蛋白热量一般取决于病人的静息能量消耗及其活动情况,一般对于无严重感染或烧伤的病人,提供30~35Kcal/(kg.d)的非蛋白热量较为理想,其中15%~40%的非蛋白热量可由脂肪乳剂提供,热氮比一般为100—150:1。 4.目前常用肠内营养制剂中糖含量一般均较高,容易导致病人体内脂肪堆积而蛋白质合成不足,体细胞群改善不明显。可以考虑督促病人加强功能锻炼,同时添加蛋白质组件以弥补蛋白质的不足,减少糖的摄入。或考虑使用以缓释淀粉为碳水化合物的肠内营养制剂以减少单位时间内的糖摄入。 5.根据病人的消化吸收能力,确定肠内营养配方中营养物质的化学组成形式。消化功能受损(如胰腺炎、腹部大手术后早期、胆道梗阻)或吸收功能障碍(广泛肠切除、炎症性肠病、放射性肠炎)者,需要简单、易吸收的配方(如水解蛋
肠外与肠内营养临床应用原则 (摘自ASPEN “Guideline for the use of parenteral and enteral nutrition in adult and pediatric patients ”) 前言 ASPEN(美国肠外与肠内营养学会)曾在1993年出版了“肠外与肠内营养临床应用原则”,旨在为临床营养支持提供一个指导性的规范,1999年ASPEN再次组织专家小组对其进行修订,并于今年年初推出了这个2002年修订版本。 临床营养的发展及其对现代医学的贡献是我们有目共睹的,在我国,近些年来临床营养的理论水平和应用水平进步也相当快,而目前我们在基层临床仍缺乏一个具有普遍指导能力的应用规范或原则,ASPEN发布的这个“肠外与肠内营养临床应用原则”为我们提供了很有价值的参考,然而我们仍然非常需要一个针对中国临床符合中国国情的“临床营养应用原则”,希望本文,美国版的“肠外与肠内营养临床应用原则”的摘要译文,为广大中国临床医生提供临床营养的参考指导的同时,能早日呼唤出相应的“中国版本”,以促进我国的临床营养事业的进一步发展。 “肠外与肠内营养临床应用原则”的3个目标: 1.必须真实地反映出营养支持在目前临床实践及研究中的最新进展; 2.必须为临床医生及专业从事营养支持的医务人员提供表述清晰、具有临床实践依据的建议指导; 3.将作为一种工具,为政策制定者、健康卫生机构、保险公司和从事临床营养的专业人员提供参考,以进一步改善医疗体系及与临床营养支持相关的政策、规定。 指导原则所依据的可靠程度分为三个级别(分别标示在下文的括号内): A. 其可靠性根据前瞻的、随机的研究结果;
肠内营养指南(适应症,禁忌,常见并发症,注意事项) 发表者:陈泽涛 3650人已访问 营养是治疗疾病和健康长寿的保证。对患者来说,合理、平衡、及时的临床营养治疗极为重要。营养治疗包括肠内营养(enteral nutrition ,EN) 治疗和肠外营养(parenteral nutrition ,PN) 治疗,而前者又分为饮食治疗和管喂营养治疗。危重病人的营养治疗非常重要,俗话说“疾病三分治,七分养”,营养即在其中。任何时候都应遵循,如果胃肠存在,就应首先考虑使用肠内营养。与肠外相比,肠内营养经济、安全、方便,符合生理过程。 为提高临床营养治疗效果,规范临床营养治疗程序,在参照国内外相关资料的基础上,结合我们的经验,制订营养治疗指南,供临床应用参考。 肠内营养指南 一、适应证 1、意识障碍、昏迷和某些神经系统疾病:如脑外伤、脑血管疾病、脑肿瘤、脑炎等所致的昏迷患者,老年痴呆不能经口进食或精神失常、严重抑郁症、神经性厌食者等; 2、吞咽困难和失去咀嚼能力:如咽下困难、口咽部外伤及手术后、重症肌无力者等; 3、上消化管梗阻或手术:如食管炎症、化学性损伤等造成咀嚼困难或吞咽困难、食管狭窄梗阻、食管癌、幽门梗阻、吻合口水肿狭窄、胃瘫等; 4、高代谢状态:如严重创伤、大面积烧伤、严重感染等所致机体高代谢、负氮平衡者; 5、消化管瘘:通常适用于低流量瘘或瘘的后期,如食管瘘、胃瘘、肠瘘、胆瘘、胰瘘等。对低位小肠瘘、结肠瘘及空肠喂养的胃十二指肠瘘效果最好; 6、术前准备和术后营养不良:如术前肠管准备期间、术中有额外营养素丢失者等; 7、炎性肠管疾病:如溃疡性结肠炎、Crohn s 病等; 8、短肠综合征:短肠综合征肠代偿阶段; 9、胰腺疾病:急性胰腺炎肠功能恢复后、慢性胰腺功能不全者。注意喂养管应插入近端空肠10cm 以上,营养制剂只能选用小分子低脂不需要消化即可吸收的要素膳,如维沃、爱伦多、大元素等; 10、慢性营养不足:如恶性肿瘤、放疗、化疗患者及免疫缺陷疾病者等; 11、器官功能不全:如肝、肾、肺功能不全或多脏器功能衰竭者; 12、某些特殊疾病:急性放射病,各种脏器移植者,包括肾移植、肝移植、小肠移植、心脏移植、骨髓移植等; 13、肠外营养治疗不能满足要求时的补充或过渡。 二、禁忌证 1、完全性机械性肠梗阻、胃肠出血、严重腹腔感染; 2、严重应激状态早期、休克状态、持续麻痹性肠梗阻; 3、短肠综合征早期; 4、高流量空肠瘘; 5、持续严重呕吐、顽固性腹泻、严重小肠炎、严重结肠炎; 6、胃肠功能障碍,或某些要求胃肠休息的情况; 7、急性胰腺炎初期; 8、3 个月以内婴儿、严重糖类或氨基酸代谢异常者,不宜使用要素膳。 三、并发症 (一)胃肠并发症 1、恶心、呕吐:主要是因有些营养液,高渗透压导致胃潴留,输注速度过快,乳糖不耐受,营养液脂肪含量过高等,特别是要素膳的口感差。可按上述病因,作相应处理,要素膳推荐
肠外营养 1.肠外营养输注途径指南 [背景]用于肠外营养输注的静脉臵管途径可分为周围静脉导管(PVC)与中心静脉导管(CVC)。中心静脉臵管又可分为经外周穿刺臵入中心静脉导管(PICC)、直接经皮穿刺中心静脉臵管、隧道式中心静脉导管(CVTC)、输液港(Port)。选择何种输注途径,需考虑以下因素:患者以往静脉臵管病史,静脉解剖走向,出凝血功能,预计PN持续时间,护理环境,潜在疾病等1。中心静脉臵管(CVC)的应用越来越普遍,包括肠外营养液输注,血制品输注等。应用CVC可显著减少周围静脉穿刺次数。但不可避免地也会引起某些并发症。因此,必须由经培训的专门人员臵管和维护,操作时必须严格遵守无菌操作规则。 [证据] 1)输液途径选择周围静脉臵管定义为皮下浅静脉臵短导管或钢针。美国静脉输液护理学会(INS)组织编写并发表的《输注治疗护理实践标准》中提出超过10%葡萄糖和/或5%蛋白质的肠外营养液,pH值<5或>9 的液体/药物,以及渗透压大于500mosm/L的液体/药物,不适合经周围静脉输注。但目前临床广泛使用的全合一营养液,含有脂肪乳剂,不仅能够有效降低溶液渗透压,还有一定的保护血管内皮作用。此外,长时间均匀慢速输注也能够减少对血管刺激。有作者报道,不超过900mosm/L渗透压的静脉营养液可经周围静脉输注。20世纪90年代期间,有关经周围静脉输注肠外营养液的前瞻性研究得到较
为一致的结论为70%以上患者周围静脉能够耐受常规能量与蛋白质密度的肠外营养配方全合一溶液,但输注肠外营养超过10~14d后,周围静脉较难耐受。 中心静脉臵管途径包括锁骨下静脉穿刺、颈内静脉穿刺、股静脉穿刺。需长期使用,还可采用有隧道式中心静脉导管(如Broviac CVC 和Hickman CVC)。经周围中心静脉臵管(PICC)是自20世纪90年代发展起来的新的静脉穿刺技术,注册护士经培训合格,即可操作。 迄今有关PICC的RCT研究较少。2000年发表的1项比较PICC与CVC 的随机对照研究[ 5]结果显示PICC的血栓性静脉炎发生率较高,穿刺难度更高,穿刺未能达到预计部位的发生率更高,但感染、导管异位、导管堵塞的发生率两者间差异无显著性。其他几个非RCT研究同样报道PICC臵管难度较高,且局部并发症、导管断裂/渗漏的发生率较高,而感染性并发症发生率与CVC比较有减少趋势。至2003年,1 项前瞻性多中心调查研究结果显示,PICC感染发生率较CVC更低。2005年发表的1篇队列研究结果提示,与颈内及锁骨下静脉穿刺相比(感染率2~5例/1000导管臵管日),PICC感染率无显著差异(2.1例/1000导管臵管日),但高于隧道式中心静脉导管(1例/1000导管臵管日)。近年来临床应用PICC越来越广泛,随着穿刺与护理经验的不断积累,以及PICC导管自身技术改进,并发症的发生率有下降趋势。迄今没有RCT 研究比较PICC与CVC的感染率。综合上述报告结果,PICC的血栓性静脉炎发生率高于CVC;而感染发生率有不同的报道结果。因此,需要综合考虑患者的病情、血管条件、可能需要的营养液输注天数、操作
肠外肠内营养临床指南(2006 版) 第一部分总论 第二部分成人营养需要量 第三部分营养风险筛查(NRS) 第四部分肠外营养素 第五部分输注路径 第六部分疾病营养支持 一.术后糖电解质输液 二.围手术期肠外营养 三.围手术期肠内营养 四.危重病 五.成人烧伤 六.胰腺炎 七.短肠综合征与胃肠道瘘 八.炎性肠病 九.肝脏疾病与肝移植 十.心血管疾病 十一.神经性疾病 十二.糖尿病
Ⅱ.肠外肠内营养临床指南(2006 版) 第一部分总论 中华医学会肠外肠内营养学分会(Chinese Society of Parenteral and Enteral Nutrition, CSPEN)于2004年12月在京成立。作为一个多学科学术组织,CSPEN的愿景(vision)是倡导循证营养实践,促进我国肠外肠内营养的合理应用,为患者提供安全、有效和具有良好效价比的营养治疗。编写、制定与推广临床指南是实现上述目标的重要途径。指南定义为:按照循证医学原则,以当前最佳证据为依据,按照系统和规范方法,在多学科专家、大中规模医院的临床医师和护理人员合作下达成的共识。 本指南的宗旨是为临床医师、护理工作者、营养师和患者在特定临床条件下,制定和/或接受肠外肠内营养治疗方案提供帮助,并为卫生政策的制定者提供决策依据。 2005年,CSPEN组织我国临床营养、儿科、外科、内科等多学科专家成立了第一届《肠外肠内营养指南》编写委员会,于当年制定和公布了第一版《肠外肠内营养学临床―指南‖系列一:住院患者肠外营养支持的适应证》,先后在《中国临床营养杂志》、《中华医学杂志》和《中华外科杂志》登载。这是我国首个按照循证医学原则制定的肠外肠内营养指南,出版后受到国内同行的关注。 2006年版指南制订过程 在2005年版的基础上,2006年1月,CSPEN开始组织《肠外和肠内营养临床指南》修订工作。在广泛听取和收集国内同行意见和建议的基础上,2006年4月,召开了2006版指南第一次“共识工作会议”,讨论重症患者应用营养支持的共识。2006年5月27日,CSPEN 在武汉召开了第二次―共识工作会议‖,讨论营养输注系统共识。裘法祖院士出席了本次会议,并且就指南编写的意义和方向做了指导,建议定期修订和核对,及时开展普及教育工作。 来自肠外肠内营养、儿科、外科、内科、护理、肿瘤科、烧伤科等专业的52位专家和部分二级医院的医师和护士,组成8个编写组,分别进行指南草案的制定和修订工作。 4月至8月间,有七个编写组先后召开了九次―共识‖会议。就本版指南的结构、证据分级和推荐意见分级,以及文献检索策略等方法学问题展开讨论,确定了工作方案,并就完成共识编写的时间表达成一致。 各组完成的共识提交至编写委员会支持小组。由支持小组统稿后,经2006年9月2日常委审稿会审查后,完成指南(草案)。 指南(草案)提交中华医学会肠外肠内营养学分会常委,并于2006年9月14日召开CSPEN
临床肠内及肠外营养操作指南 (草案) 中华外科学会临床营养支持学组 2004.3 目录 第一章概述(吴肇汉) (1) 第二章营养评价(曹伟新) (4) 第三章成人的正常营养需要(徐鹏远) (8) 第四章肠内及肠外营养 (12) 第一节肠内营养(李宁) (12) 第二节肠外营养(于健春) (14) 第三节肠内及肠外营养并发症(林锋) (17) 第五章药物与营养素的相互作用(吴国豪) (19) 第六章各种疾病的营养支
持 (22) 第一节老年人(王为忠) (22) 第二节心脏病(林锋) (23) 第三节肺部疾病(许媛) (25) 第四节糖尿病(徐鹏远) (26) 第五节肾衰竭(刘敦贵) (28) 第六节肝硬化(迟强) (30) 第七节脑损伤(朱维铭) (31) 第八节烧伤(伍晓汀) (33) 第九节危重病人(许媛) (34) 第十节胃肠功能衰竭(彭俊生) (35) 第十一节短肠综合征(吴肇汉)…………………………
37 第十二节胰腺炎(伍晓汀) (39) 第十三节炎性肠道疾病(王为忠) (40) 第十四节消化道瘘(李宁) (42) 第十五节癌症(曹伟新) (44) 第十六节器官移植(刘敦贵) (45) 第十七节围手术期(周岩冰) (46) 第七章常用EN及PN制剂(朱维铭) (47) 第一章概述 临床营养支持的研究和实施已经有30余年的历史。早在20世纪60~70年代,曾宪九、黎介寿,吴肇光等前辈就深切意识到营养支持 在外科的重要意义。尽管当时药品和器材都极为匮乏,仍然带领我们开展了这项工作。经过数十年的努力,临床营养支持的理念不仅被广大医
学界所接受,而且它已经成为救治各种危重病人的重要措施之一,挽救了无数病人的生命。改革开放以来,引进了相当多的优质产品和器材, 而且逐步已在国内生根、开花,这又为我们开展临床营养支持创造了更好的条件。现在可以毫不夸张地说,在全国各大教学医院里,特别是某 些领先的单位,临床营养治疗的水平已经基本达到国际先进水平。 但是,我国幅员广大,各地区发展的不平衡在所难免。在边远地区,受条件的限制而发展较慢。由于疾病谱的关系,各地区、各 单位所能积累到的经验也会有所不同。例如,国内大多数的肠瘘病人都集中在南京军区总医院,原发性肝癌和肝移植也是集中在国内几家大医 院里。这些医院很容易积累治疗这类病人的经验,而其他医院则很缺乏这种临床体验。另外,虽然临床营养支持治疗首先是从普外科“起家” ,但显然这项措施是适合整个临床医学的各个领域,而不是仅仅局限在外科。但从目前情况看,其他学科对营养代谢的认识还显得不足,营养
1 ICU 肠外肠内营养支持指南流程图(EN )1表:CSPEN-ICU 否 否 否
ICU肠外肠内营养支持指南流程图(EN)2表:CSPEN-ICU 肠外肠内营养支持ICU-营养制剂的选择 2
ICU肠外肠内营养支持指南流程图(EN)3表:CSPEN-ICU 3
ICU肠外肠内营养支持指南流程图(EN)4表:CSPEN-ICU 中华医学会肠外肠内营养学分会CSPEN【肠外肠内营养与危重病学协作组 CSPEN-ICU】 A. 临床营养支持;营养支持的时间(早期或晚期) 1.危重病患者,营养支持只有在生命体征稳定(血流动力学、呼吸功能稳定-包括药物、呼吸机等治疗措施控制下)情况下才能进行。(A) 2.危重病患者APACHII>10存在重度营养不良风险,需要营养支持。(A) 3.早期营养支持有助于改善危重病患者的临床结局。(A);危重病患者在入ICU后24小时~72小时开始。(C) B、营养支持途径(肠外营养支持PN或肠内营养支持EN) 4.只要胃肠道解剖与功能允许,应首选EN。(A级) 5.经胃肠道不能到达营养需要量的危重病患者,应考虑PN支持,或肠内外营养联合应用。(A级) C、营养支持部位(胃、肠道)、能量 6.危重病患者肠内营养首选经胃途径。(C);对胃内营养具有高风险的危重病患者可选择空肠营养。(A级) 7.存在严重胃潴留或胃食管反流的患者,可尝试应用辅助胃动力药物(胃复安等)改善胃肠道动力。(C) 8.短期肠外营养支持建议经周围静脉输注(B);PN支持时间预计>10~14天,建议采用CVC或PICC置管(B);中心静脉导管头部应位于上腔静脉内(A);中心静脉穿刺部位首选锁骨下静脉可能较佳(C)。―――证据及参考文献(参见导管组指南) 9.危重病患者急性应激期营养支持原则(20 - 25 kcal/kg?day);在应激与代谢状态稳定后,能量供给量需要适当的增加(25-30)。(C级)本部分编写人员:石俊;江华;何振扬;陶晔璇;王新颖;李元忠。 修改稿:2006年9月2日北京CSPEN常委会讨论通过。2006年9月14日天津全国指南工作会上:发布 4
XX医院 临床肠内及肠外营养操作指南 第一节肠内营养 【肠内营养适应证及其优点】 1.口服摄入不足,但胃肠道有消化吸收功能的病人,可以应用肠内营养支持。 2.要努力实施肠内营养支持,即使暂时不成功也要尽可能创造条件去反复尝试肠内营养,因为临床病人一旦耐受了肠内营养,将受益无穷。 3.营养物质经门静脉系统吸收输送至肝脏,有利于内脏(尤其是肝脏)的蛋白质合成及代谢调节。 4.长期持续应用全肠外营养会使小肠粘膜细胞和营养酶系的活性退化,而肠内营养可以改善和维持肠道粘膜细胞结构与功能的完整性,有防止肠道细菌易位的作用。 5.肠外营养导致内脏血流与心搏出量增加,使代谢营养物质消耗的能量增加。 6.在同样热卡与氮量的条件下,应用肠内营养的病人的体重增长、氮潴留均优于全肠外营养,而且人体组成的改善也较明显。7.肠内营养较价廉,对技术和设备的要求较低,使用简单,易于临床管理。 【肠内营养配方的选择】 1.可供临床选用的肠内营养配方很多,成分与营养价值差
别很大,选择配方时主要考虑其蛋白质、碳水化合物与脂肪 的来源及比例,各配方的膳食纤维、维生素和矿物质含量也可能不同。肠内营养制剂发展迅速,配方常有改变,因此要注意所用产品的具体配方。 2.根据病人的营养状态及代谢状况确定营养需要量,高代谢病人应选择高热卡配方,需要限制水分摄入的病人应选择浓度较高的配方(如能量密度为/ ml),免疫功能异常的病人应选择具有免疫调节作用的配方。 3.肠内营养支持提供的非蛋白热量一般取决于病人的静息能量消耗及其活动情况,一般对于无严重感染或烧伤的病人,提供30?35Kcal/的非蛋白热量较为理想,其中15% ~40%的非蛋白热量可由脂肪乳剂提供,热氮比一般为100—150:1 。 4.目前常用肠内营养制剂中糖含量一般均较高,容易导致病人体内脂肪堆积而蛋白质合成不足,体细胞群改善不明显。可以考虑督促病人加强功能锻炼,同时添加蛋白质组件以弥补蛋白质的不足,减少糖的摄入。或考虑使用以缓释淀粉为碳水化合物的肠内营养制剂以减少单位时间内的糖摄入。 5.根据病人的消化吸收能力,确定肠内营养配方中营养物质的化学组成形式。消化功能受损(如胰腺炎、腹部大手术后早期、胆道梗阻)或吸收功能障碍(广泛肠切除、炎症性肠病、放射性肠炎)者,需要简单、易吸收的配方(如水解蛋白、多肽或氨基
肠内营养指南(适应症,禁忌,常见并发症,注意事项) 发表者:陈泽涛 3650人已访问 营养是治疗疾病和健康长寿的保证。对患者来说,合理、平衡、及时的临床营养治疗极为重要. 营养治疗包括肠内营养(enteral nutrition ,EN) 治疗和肠外营养(parenteral nutrition , PN)治疗,而前者又分为饮食治疗和管喂营养治疗. 危重病人的营养治疗非常重要,俗话说“疾病三分治,七分养”,营养即在其中。任何时候都应遵循,如果胃肠存在,就应首先考虑使用肠内营养.与肠外相比,肠内营养经济、安全、方便,符合生理过程.。。.。。。文档交流 为提高临床营养治疗效果,规范临床营养治疗程序,在参照国内外相关资料的基础上,结合我们的经验,制订营养治疗指南,供临床应用参考.。。..。.文档交流 肠内营养指南 一、适应证 1、意识障碍、昏迷和某些神经系统疾病:如脑外伤、脑血管疾病、脑肿瘤、脑炎等所致的昏迷患者,老年痴呆不能经口进食或精神失常、严重抑郁症、神经性厌食者等;。。。。。。文档交流 2、吞咽困难和失去咀嚼能力:如咽下困难、口咽部外伤及手术后、重症肌无力者等; 3、上消化管梗阻或手术:如食管炎症、化学性损伤等造成咀嚼困难或
吞咽困难、食管狭窄梗阻、食管癌、幽门梗阻、吻合口水肿狭窄、胃瘫等;。.....文档交流 4、高代谢状态:如严重创伤、大面积烧伤、严重感染等所致机体高代谢、负氮平衡者; 5、消化管瘘:通常适用于低流量瘘或瘘的后期,如食管瘘、胃瘘、肠瘘、胆瘘、胰瘘等。对低位小肠瘘、结肠瘘及空肠喂养的胃十二指肠瘘效果最好;。。。。.。文档交流 6、术前准备和术后营养不良:如术前肠管准备期间、术中有额外营养素丢失者等; 7、炎性肠管疾病:如溃疡性结肠炎、Crohn s 病等; 8、短肠综合征:短肠综合征肠代偿阶段; 9、胰腺疾病:急性胰腺炎肠功能恢复后、慢性胰腺功能不全者。注意喂养管应插入近端空肠10cm 以上,营养制剂只能选用小分子低脂不需要消化即可吸收的要素膳,如维沃、爱伦多、大元素等;。.。。。。文档交流 10、慢性营养不足:如恶性肿瘤、放疗、化疗患者及免疫缺陷疾病者等; 11、器官功能不全:如肝、肾、肺功能不全或多脏器功能衰竭者; 12、某些特殊疾病:急性放射病,各种脏器移植者,包括肾移植、肝移植、小肠移植、心脏移植、骨髓移植等; 13、肠外营养治疗不能满足要求时的补充或过渡。 二、禁忌证 1、完全性机械性肠梗阻、胃肠出血、严重腹腔感染;
中国老年患者肠外肠内营养应用指南(2020) 中华医学会肠外肠内营养学分会老年营养支持学组在2013年肠外肠内营养中国老年患者专家共识基础上,组织我国老年医学、循证医学、公共卫生、临床营养领域工作的学者以及临床相关学科的专家共同合作,总结了国内外老年营养支持治疗领域出现的新证据,对共识进行全面更新并升级为指南。 一、营养支持团队 营养支持团队(NST)组成中,老年医学专家发挥协助组建和管理的作用,营养(医)师、临床药师、物理康复师和护士作为团队的主要成员,外科、口腔科、神经科、心理医学科等临床专科医师为管理团队提供技术保障。已有许多研究证实NST的存在的确能提高营养支持的效价比,尤其在降低营养支持并发症、降低住院患者的医疗费用、减少住院时间等方面发挥重要作用。NST的主要工作目标是为老年患者提供合理的营养支持,包括:(1)识别是否存在营养不良或营养风险;(2)制订合理的营养支持方案;(3)提供安全、合理、有效的营养支持;(4)监测及评价营养支持的效果。 推荐1: NST需要多学科人员构成,由老年医学专科医师牵头,建立包括临床专科护士、营养师、药师等在内的NST(证据B,强推荐,97%)。 二、确定能量与蛋白质目标 推荐2:
老年住院患者的能量需求可通过间接测热法进行个体化测定(证据C,弱推荐,90%)。一般老年患者可将20~30 kcal·kg-1·d-1作为能量供给的目标(证据B,弱推荐,96%)。老年住院患者的蛋白质需结合临床实际情况设计,每日可达到1.0~1.5 g/kg蛋白质目标摄入量,乳清蛋白制剂更易消化利用(证据C,弱推荐,82%)。 推荐3: 接受EN治疗的老年住院患者,应结合疾病状态及胃肠道耐受能力,选择适宜脂肪供能比的制剂(证据A,强推荐,99%)。推荐接受PN治疗住院老年患者的脂肪供能可适当增加(一般不超过非蛋白质热卡的50%)(证据C,弱推荐,99%)。 推荐4: 老年术后患者接受营养治疗时适当补充谷氨酰胺可减少感染并发症,同时应监测患者的肝肾脏功能并限制谷氨酰胺的剂量(≤0.5 g·kg-1·d-1)(证据B,弱推荐,97%)。住院老年患者可考虑在药理范围内补充ω-3脂肪酸,可能具有改善临床预后的作用(证据C,弱推荐,92%)。 三、营养筛查与评价 推荐5: 老年患者营养不良发生率高,推荐常规进行营养筛查;推荐MNA-SF和NRS2002营养筛查工具(证据A,强推荐,97%)。