ORIGINAL RESEARCH PAPER
Reduced apoptosis correlates with enhanced autophagy in synovial tissues of rheumatoid arthritis
Ke Xu ?Peng Xu ?Jian-Feng Yao ?Yin-Gang Zhang ?
Wei-kun Hou ?She-Min Lu
Received:12April 2012/Revised:15October 2012/Accepted:25October 2012/Published online:20November 2012óSpringer Basel 2012
Abstract
Objective Defective apoptosis contributes to the massive synovial hyperplasia in rheumatoid arthritis (RA),but the mechanism is largely unknown.To investigate the reasons for the reduced apoptosis in RA synovium,we analyzed autophagy and its relationship to apoptosis in synovial tissues from RA and osteoarthritis (OA)patients.
Methods Synovial tissues were obtained from seven RA and 12OA patients undergoing knee replacement surgery.Apoptosis was detected by the terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL)assay and staining for p85fragment of PolyADP-ribose polymerase (PARP).Autophagy was determined by immunoblotting for the autophagic markers Beclin-1and LC3.MicroRNA-30a (miR-30a),which targets Beclin-1,was measured by real-time RT-PCR.The interplay between autophagy and apoptosis was determined via Spearman’s correlation analysis.
Results In comparison with OA,the synovial tissues from RA displayed decreased TUNEL-positive nuclei
(P \0.01).In contrast,Beclin-1and LC3were overex-pressed in the synovial lining layers of RA,which was correlated with decreased levels of miR-30a.Moreover,there was a signi?cant reverse relationship between apop-tosis and autophagy in RA synovial tissues (P \0.01and r =-0.8937).
Conclusion The impaired apoptosis in RA synovium might result from increased autophagy,which in turn could be due to the deregulation of miRNA-30a.Keywords Rheumatoid arthritis áOsteoarthritis áAutophagy áApoptosis áSynovium
Abbreviations H&E Hematoxylin–eosin OA Osteoarthritis OD Optical density PARP PolyADP-ribose polymerase RA Rheumatoid arthritis SF Synovial ?broblast TBST Tris-buffered saline with Tween 20TUNEL Terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling
Introduction
Synovial hyperplasia,chronic in?ammation,and autoim-mune reaction are the major histological features of rheumatoid arthritis (RA)[1],and the hyperplasia is the driving force behind the in?ammatory and destructive responses [2].Accumulating data indicate that the massive synovial hyperplasia of RA results from defective (reduced)apoptosis [3,4];apoptosis is rarely found in the synovial tissues of either RA patients or animal models of
Responsible Editor:John Di Battista.
K.Xu áP.Xu (&)áJ.-F.Yao áW.Hou
Department of Joint Surgery,Hong Hui Hospital,Xi’an Jiaotong University College of Medicine,Xi’an 710054,China e-mail:sousou369@https://www.doczj.com/doc/041366795.html,
Y.-G.Zhang
Department of Orthopedics,First Af?liated Hospital of Xi’an Jiaotong University College of Medicine,Xi’an 710061,China S.-M.Lu (&)
Department of Genetics and Molecular Biology,Xi’an Jiaotong University College of Medicine,Xi’an 710061,China e-mail:lushemin@https://www.doczj.com/doc/041366795.html,
In?amm.Res.(2013)62:229–237DOI 10.1007/s00011-012-0572-1
In?ammation Research
RA,and RA synoviocytes evaded apoptosis in vitro[5–9]. However,the mechanisms that account for reduced apop-tosis in RA synovium are not de?nitively known.
It is widely accepted that there exists a complex inter-play between the processes that regulate autophagy and apoptosis[10,11].Autophagy is a survival strategy for cells undergoing nutrient deprivation or other stresses,and it plays an important role in the development of many diseases such as cancers and neurodegenerative diseases [12–14].The proteins Beclin-1and microtubule-associated protein(MAP)-light chain3(LC3)are critical to the autophagic process[15,16].Beclin-1,the mammalian homolog of the yeast Atg6,controls the death and survival of various types of cells and promotes autophagy[17,18]. LC3is a component of autophagosomes and has two forms, LC3-I(18kDa)and LC3-II(16kDa).The cytoplasmic LC3-I is processed,recruited to the autophagosomes,and converted to LC3-II via site-speci?c proteolysis and lipi-dation[19].Thus,LC3-II is a reliable marker of autophagy [20].
Recent studies with RA patients demonstrated that autophagy protects cells from death by limiting the ER stress response in?broblasts[21].This suggests that in synovial tissues from RA patients autophagy is upregu-lated,and reduced apoptosis may be due to hyperactive autophagy.However,these data were obtained from cul-tured synovial?broblasts,which may not be representative of all in?ammatory cells and can not re?ect the actual level of autophagy in situ.In the present study,we used synovial tissues from RA patients to detect the levels of apoptosis and autophagy and analyzed the association between apoptosis and autophagy.Interestingly,we found that there was decreased expression of miRNA-30a,which targets Beclin-1.Our data suggest that the hyperactive autophagy in RA might result from decreased expression miRNA-30a.
Materials and methods
Human tissue collection and processing
Synovial tissues were obtained from seven RA and12 osteoarthritis(OA)patients undergoing knee replacement surgery.Clinical data,laboratory examination and medi-cations of patients are summarized in Table1.All patients gave informed written consent for isolation of synovial tissues.Each specimen was divided into two parts;one part was immediately preserved in liquid nitrogen for30min for Western blot and real-time PCR assays,and the other was?xed in4%paraformaldehyde(in normal saline)for immunohistochemistry.All tissue samples were veri?ed by hematoxylin–eosin(H&E)staining.The experiment was approved by the ethics committee of Hong Hui Hospital, Xi’an Jiaotong University College of Medicine.
Terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling(TUNEL)assay
Tissue sections were transferred to xylene and rehydrated in an alcohol series.The samples were then covered with 50l L of proteinase-K solution and incubated at room temperature for15–30min.Endogenous peroxidase activity was inactivated by3%H2O2.The TUNEL assay was performed using a kit(Trevigen,MD,USA)according to the manufacturer’s instructions.
Positive controls were obtained by incubating?xed and permeabilized sections with DNase-I.Negative controls omitted the terminal deoxynucleotidyl transferase labeling reaction mixture and terminal deoxynucleotidyl transferase,to prevent the potentially inappropriate inclusion of nucleotides. Four randomly chosen?elds per section with at least100cells were examined at high magni?cation(initial magni?cation 4009)to calculate the percentage of TUNEL-positive nuclei. Total RNA isolation,cDNA synthesis,stem-loop
RT-PCR and real-time PCR
Total RNA was extracted from OA and RA synovial tissues with TRIzol reagent(Invitrogen,Carlsbad,CA,USA)by following the manufacturer’s instructions.The total RNA was examined via electrophoresis on a1%agarose gel, and the quantity was determined based on the absorbance at260nm(A260).Finally,the RNA was analyzed for purity according to the ratio of optical density(OD)at260 and280nm(A260/A280);only samples with an OD ratio Table1Characteristics of patients
Patients RA OA Number712
Age(years)*57(43*65)64(48*73) Gender(female/male)5/210/2
CRP(mg/L)# 4.05(2.11) 1.21(1.06) RF(positive/total)7/71/12
ESR(mm/h)#24(6)3(2)
DAS28# 2.03(0.17)NA Medications(number)MTX(2)DSSRC(12)
MTX/TWP(3)
TWP(2)
CRP C-reactive protein,DAS28disease activity score28,DSSRC diclofenac sodium sustained release capsules,ESR erythrocyte sedi-mentation rate,MTX methotrexate,NA not available,RF rheumatoid factor,TWP Tripterygium wilfordii polyglycoside
*Median(range)
#Mean(SEM)
230K.Xu et al.
1.7–
2.0were selected.A two-step reverse transcription (RT)PCR was conducted.The?rst-strand cDNA was synthesized from2.5l g of total RNA with avian myelo-blastosis virus reverse transcriptase(Takara,Tokyo, Japan).
To establish the reference standards for real-time PCR, Beclin-1,LC3,and b-actin were ampli?ed using speci?c primers(Table2).PCR was performed on an MJ Research PTC-200thermal cycler(MJ Research,USA)in a20l L reaction system containing10l L29SYBRògreen I mix (Takara,Tokyo,Japan).All real-time PCR assays were performed in triplicate with Bio-Rad iQ5multicolor real-time PCR detection system(Hercules,CA,USA)in accordance with the manufacturer’s protocol.Following a denaturation at95°C for5min,PCR was carried out for 40reaction cycles with a melting temperature of95°C for 30s,annealing temperature of60°C for30s,and an extension temperature of72°C for1min.A?nal elonga-tion at72°C for30min was preformed.The amplicons were examined on a1%agarose gel after electrophoresis. Data analysis was performed with the sequence detector system software.The relative quantity was calculated by the DD Ct method,with b-actin as the housekeeping gene. The results were assessed with the t test.
MicroRNA-30a expression was determined using the stem-loop RT-PCR method.U6small nuclear RNA was the internal control.The stem-loop RT primer and real-time PCR primers were designed and synthesized by RiboBio(Guangzhou,China).The relative quantity was calculated by the DD Ct method with U6and the results were assessed with the t test.
Western blot
Synovial samples from OA and RA patients were homogenized in a polytron tissue grinder(Kinematica, Bohemia,NY,USA)in lysis buffer(50mM Tris–HCl pH 7.4,150mM NaCl,0.2mM EDTA,1%Triton X-100, 1%sodium deoxycholate,0.1%SDS)and protease inhibitor cocktail(Beyotime,Shanghai,China),and then clari?ed via centrifugation at10,0009g for5min.Coo-massie brilliant blue staining was used to determine protein quality.The protein concentrations were determined with a bicinchoninic acid reagent assay(Beyotime,Shanghai, China).Forty micrograms of protein was loaded into each lane of a6,10and15%SDS gel and subjected to PAGE.
Protein was transferred to0.45l m polyvinylidene ?uoride membranes and blocked with5%dry milk in Tris buffered saline–Tween-20(TBST),and then incubated serially with rabbit polyclonal anti-PARP p85(1:1,000, Epitomics,USA),mouse polyclonal anti-Beclin-1 (1:1,000)and rabbit polyclonal anti-LC3(1:1,000)at4°C overnight.The membranes were then incubated with horseradish peroxidase-conjugated anti-mouse and anti-rabbit secondary antibody IgG(Bioss,Beijing,China)for 1h.After the incubation with secondary antibody,the membranes were washed three times with TBST and developed via electrochemiluminescence(ECL)plus Western blotting detection system.b-actin(1:1,000,Santa Cruz,USA)was used as the loading control. Immunohistochemistry
Paraf?n-embedded samples were?rst deparaf?nized in the xylene substitute Pro-Par Clearant(Anatech)and rehy-drated in graded ethanol and water.For antigen unmasking, sections in10mM sodium citrate buffer(pH6.0)were heated in a microwave oven and kept at85–90°C for 1min.Slides were cooled for20min at room temperature after antigen unmasking.After washing with PBS,the sections were blocked with5%goat serum for30min at room temperature.Antibodies for probing PARP p85 (1:80,Promege,USA),Beclin-1(1:100,Abnova,Taiwan), LC3(1:100,Sigma,USA),and the negative control PBS were applied to the slides and incubated at4°C overnight. After washing with PBS,sections were treated with3% H2O2for10min,washed with PBS,and incubated with biotinylated goat anti-mouse and goat anti-rabbit secondary antibodies at room temperature for30min.Then the sec-tions were processed using a Vectastain ABC-AP kit for another30min(Vector,Burlingame,CA,USA).The slides were washed,and the sections were incubated with 3,30-diaminobenzidine substrate for2–3min and counter-stained with hematoxylin.Beclin-1and LC3in the synovial
Table2Primers used for real-time PCR
Name Sense or antisense Sequence(50–30)Ampli?ed length(bp)Annealing temp(°C)
Beclin-1Sense GGATGGATGTGGAGAAAGGCAAG15258 Antisense TGAGGACACCCAAGCAAGACC
LC3Sense CGGAAGCCTTTTACTTGCTG18361 Antisense GTCTGTCCTCAAGGCTGCTC
b-actin Sense ATCGTGCGTGACATTAAGGAGAAG17961 Antisense AGGAAGGAAGGCTGGAAGAGTG
Enhanced Autophagy in RA231
lining layer was assessed systematically by counting positive cells in 50950l m grids.This was repeated a minimum of three times for each section.Transmission electron microscopy
Surgically resected synovial tissue samples from RA patients were ?xed in ice-cold 2%glutaraldehyde/0.1M phosphate buffer (pH 7.2),post-?xed in 1%osmium tetroxide,washed,dehydrated with graded ethanol series (30,50,70,90,and 100%),and ?nally embedded in 1:1propylene oxide/embedding resin.The resin blocks were cut with a LKB-V (LKB,Sweden)ultramicrotome.Thin (60nm)sections were picked up on 200-mesh copper grids and stained with uranyl acetate and lead citrate.The sec-tions were examined with a H-7650transmission electron microscope (HITACHI,Ibaraki,Japan).
Statistical analysis
The difference between two groups was evaluated by t test and the correlation analysis was used to assess the association between apoptosis and autophagy.The results were presented as mean ±standard deviation (SD).A P value \0.05was considered signi?cant.
Results
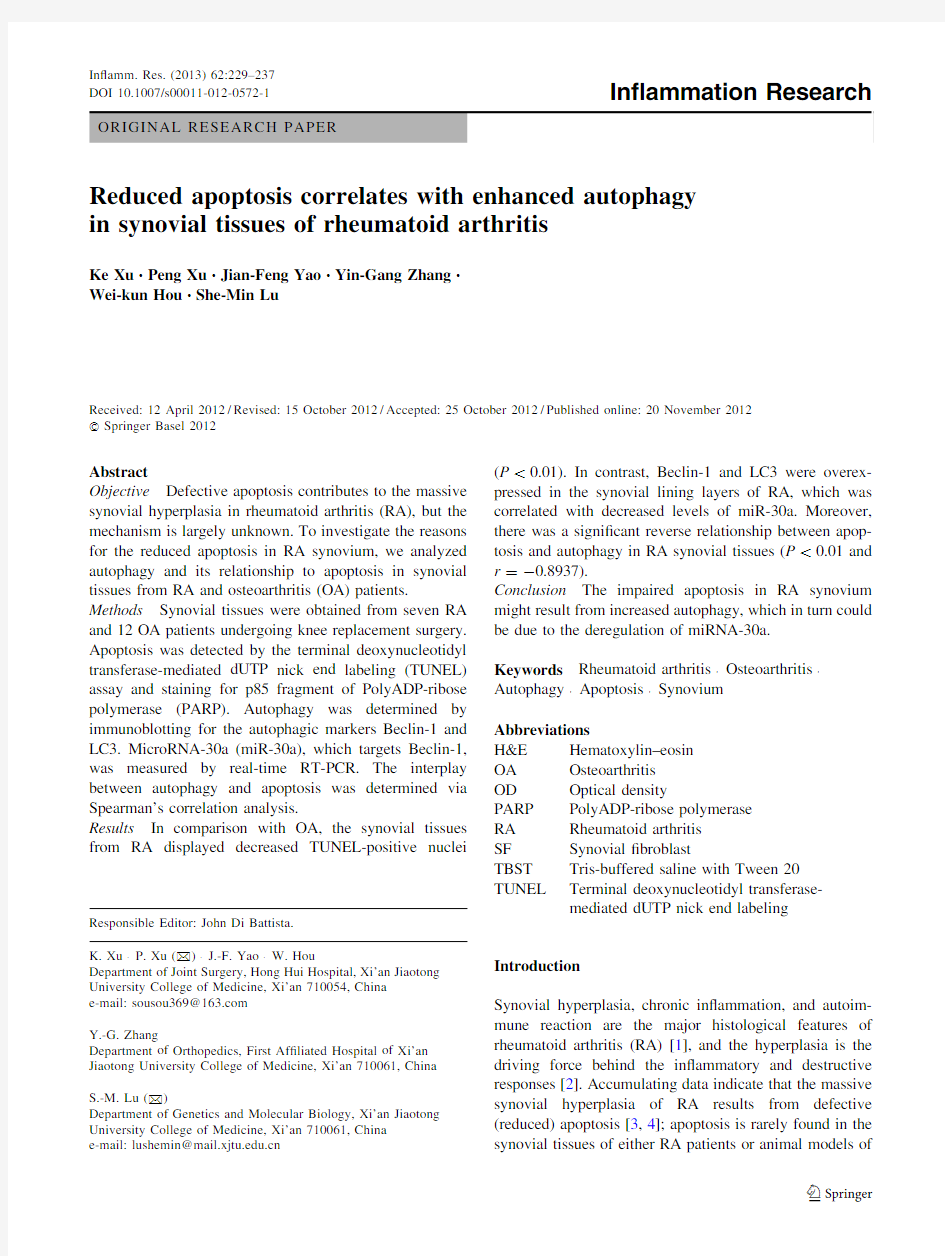
Reduced apoptosis in synovial tissues of RA
Hematoxylin and eosin staining and the TUNEL assay were performed on synovial tissues from RA and OA patients (Fig.1).Similar to previous reports [22],the thickened synovium and the in?ltration of in?ammatory
A E
PAPP p85
C TUNEL HE stain B F
D G
TUNEL
0.2
0.3
H
PARP p85
OA
RA
c e l l p e r c e n t a g e e
RA
OA
A C E
B D F 232K.Xu et al.
cells were observed in RA synovial tissues (Fig.1b).The TUNEL-positive (apopotic)and TUNEL-negative nuclei brown and blue,respectively.In OA synovial tissues,the TUNEL-positive cells were located both in the synovial lining and sublining layers.In contrast,in the RA synovial tissues,the TUNEL-positive cells were distributed mainly in the sublining layers (Fig.1c,d).Furthermore,a signif-icantly higher percentage of TUNEL-positive cells was observed in the OA synovial tissues compared with the RA (Fig.1g;P \0.01).Similar results were seen for PARP p85staining (Fig.1e,f)and Western blot of PARP p85(Fig.1h).These results demonstrated that there was reduced apoptosis in the synovial tissues of RA patients.Enhanced autophagy in RA synovial tissues
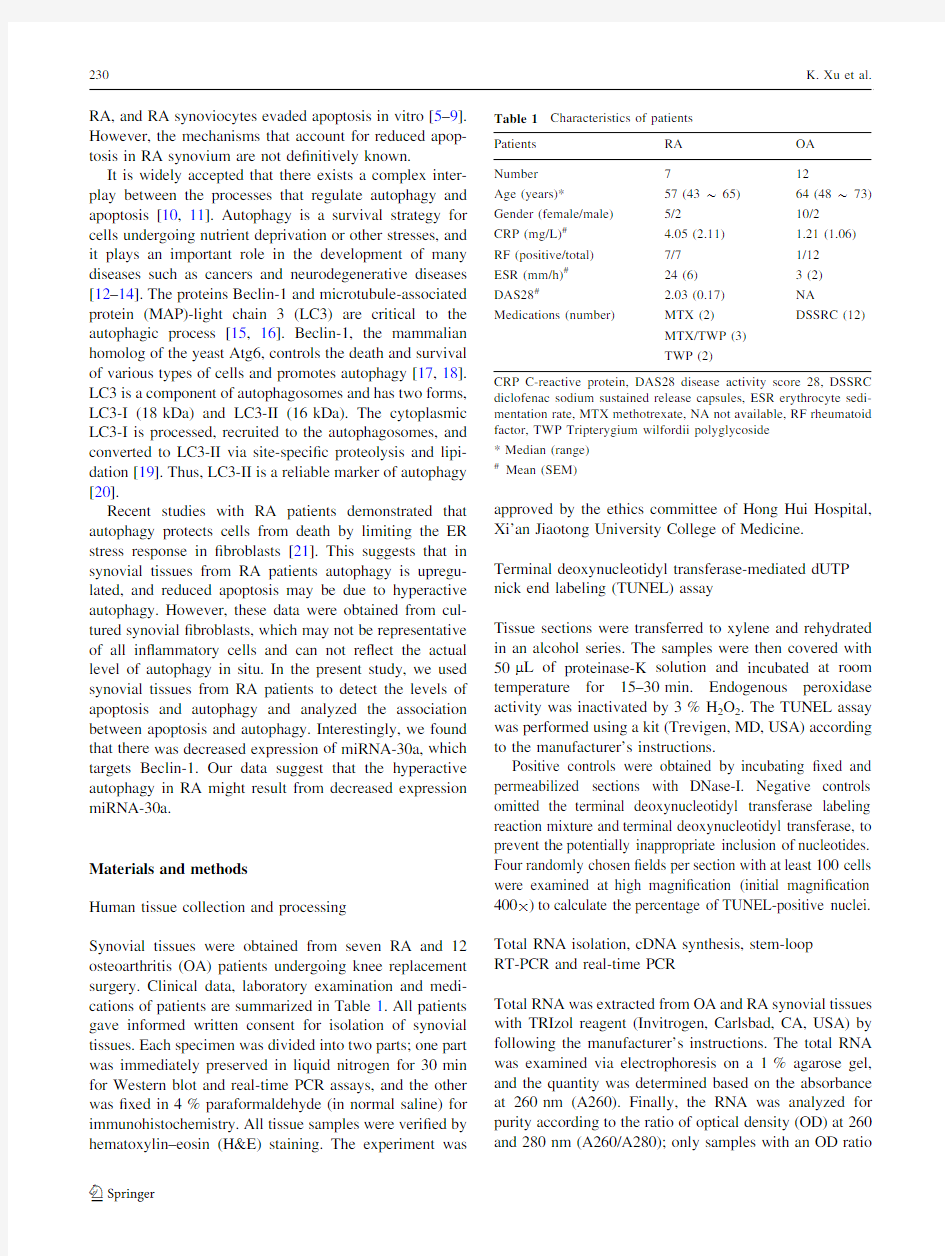
To check the status of autophagy,we tested synovial tis-sues from RA and OA patients for Beclin-1and LC3expression via real-time PCR and Western https://www.doczj.com/doc/041366795.html,pared with OA,there were signi?cantly higher levels of Beclin-1mRNA in RA synovial tissues (Fig.2a,left;P \0.01),while no signi?cant difference in the mRNA levels of LC3was observed between the synovial tissues of the two groups (Fig.2a,right;P [0.05).The increased mRNA expression of Beclin-1suggests enhanced autophagy in RA.The Western blot results also demonstrated that in comparison to OA,the RA synovial tissues had
signi?cantly higher levels of the proteins Beclin-1and LC3-II (Fig.2b;P \0.01).Thus,RA synovial tissues have an increased level of autophagy.
Beclin-1and LC3are primarily located in the synovial lining layers of synovial tissues
To determine the distribution of the autophagic markers Beclin-1and LC3in OA and RA synovial tissues,immu-nohistochemistry and H&E staining methods were applied.Beclin-1and LC3were mainly distributed in the cells of the synovial lining layer of both OA and RA patients (Fig.3C–F).To check whether the presence of LC3re?ects autophagosome formation,an LC3-positive RA specimen was examined with transmission electron microscopy.RA-SFs contained lipid bilayer structures engul?ng organelles in the cytoplasm,which are characteristic for autophagosomes (Fig.3i).Again,we observed that Beclin-1and LC3were more highly expressed in RA synovial tis-sues than OA (Fig.3j,k;P \0.01).These results indicated that autophagic markers were mainly distributed in the cells of the synovial lining layer of synovial tissues.Decreased expression of miR-30a in RA synovial tissue The increased levels of Beclin-1mRNA may explain,at least in part,the enhanced autophagy found in RA
synovial
Fig.2Increased autophagy in RA synovial tissues compared with those of OA.a The quanti?cation of mRNA levels of Beclin-1and LC3determined by real-time qPCR and normalized against b -actin.Values are the means and SDs (n =12for OA,n =7for RA).*
P \0.05and **P \0.01compared with OA synovial tissue.b Representative blots of Beclin-1,LC3,and b -actin detected via Western blot.c Relative grayscale value analysis of Beclin-1and LC3II levels corrected for b -actin.Values are the means and SDs (n =8for OA group and n =7for RA group).*P \0.05and **P \0.01compared with OA synovial tissue
Enhanced Autophagy in RA 233
tissues.To explore the mechanism underlying the increased Beclin-1mRNA and hence autophagy in RA synovial tis-sues,we utilized real-time PCR to analyze the expression of miR-30a,which targets Beclin-1,in synovial tissues of both patient groups.Quantitative analysis of real-time PCR using the DD Ct method showed a signi?cant decrease of miR-30a in RA synovial tissues (P \0.01)when compared with OA (Fig.4a).In addition,the level of miR-30a was inversely correlated with that of Beclin-1mRNA (Fig.4b,P \0.01and r =-0.6176).These results showed that there was a decrease in miR-30a expression in RA synovial tissues,which may have led to the increase of Beclin-1.
Inverse relationship between apoptosis and autophagy in synovial tissues
We investigated the association between apoptosis and autophagy in OA and RA synovial tissues with a correlation analysis of the percentage of apoptotic cells (determined via TUNEL assay)and the expressions of the autophagic markers Beclin-1and LC3-II.We found that the percentage of apop-totic cells was negatively correlated with Beclin-1(Fig.5a,P \0.05and r =-0.7404)and LC3-II (Fig.5b,P \0.01and r =-0.8937).Moreover,a signi?cant positive correla-tion was found between the percentage of apoptotic cells
and
Fig.3Beclin-1and LC3are mainly distributed in the synovial lining layers of synovial tissues.H&E-stained sections representative of OA (a )and RA (b )synovial tissues.Immunohistochemical representative assays of Beclin-1(brown stain )in OA (c )and RA (d )synovial tissues.Immunohistochemical representative assays of LC3(brown stain )in OA (e )and RA (f )synovial tissues.Negative controls using PBS in OA (g )and RA (h )synovial tissues.i Ultrastructure representative of RA synovial tissues.A macrophage (upper )and a RA-SF (lower left )from RA synovial lining layer.Original magni?cation 8,000.Asterisk indicated lipid bilayer struc-tures engul?ng organelle (lower right ).Nucl nucleus.Original magni?cation 30,000.Quanti?cation of cells positive for Beclin-1(j )and LC3(k )in synovial lining layers.Nuclei were stained with hematoxylin.Values are the means and SDs (n =12for OA group and n =7for RA group).*P \0.05and **P \0.01compared with OA synovial tissue.Scale bar =100l m (color ?gure online)
234K.Xu et al.
miR-30a expression (Fig.5c,P \0.01and r =0.6749).These results demonstrated an inverse relationship between apoptosis and autophagy in these synovial tissues.
Discussion
Hyperplasia of the synovial lining and the in?ltration of in?ammatory cells in the sublining are the typical
pathological changes of RA,and compromised apoptosis exerts an important in?uence on both.In RA synovial ?broblasts (SFs),mainly localized to the layers of the synovial lining or at the sites of cartilage invasion,are resistant to apoptosis.Apoptotic rates that are lower than normal are considered the immediate cause of synovial hyperplasia [3,23,24].Moreover,such impaired apoptosis in in?ltrating in?ammatory cells as B-and T-cells can aggravate joint in?ammation and enhance the resistance
of
Fig.4Downregulation of miR-30a in RA synovial tissues.a Quan-ti?cation of miR-30a determined by real-time qPCR and normalized against U6.Values are the means and SD (n =12for OA group and n =7for RA group).*P \0.05and **P \0.01compared with synovial tissue of OA.b Scattergraph demonstrating the inverse correlation between miR-30a and Beclin-1.r ,Spearman’s correlation coef?cient;P \0.05is statistically
signi?cant
Fig.5Correlation analysis of apoptosis and autophagy.
a Correlation between TUNEL-positive (apoptotic)cells and the relative grayscale values of Beclin-1.
b Correlation between TUNEL-positive cells and relative grayscale values of LC3-II.
c Correlation between TUNEL-positive cells an
d th
e expression o
f miR-30a.r ,Spearman’s correlation coef?cient;P \0.05is statistically signi?cant
Enhanced Autophagy in RA 235
SFs to cell death[23–27].Thus it can be concluded that insuf?cient apoptosis of synovial cells plays a pivotal role in the pathological process of RA.
Accordingly,in recent years there has been intense interest in elucidating the mechanisms of reduced apoptosis in RA synovium.Given the interplay between the two processes,it is intriguing to postulate that deregulation of autophagy may contribute to impaired apoptosis in RA [28–31].To the best of our knowledge,this is the?rst report that demonstrates increased autophagy,and the inverse association between this increase and apoptosis in synovial tissues from RA patients.
In this study,we demonstrated that in RA synovial tis-sues the autophagic markers Beclin-1and LC3were overexpressed,and LC3-1was converted to LC3-II.This suggests enhanced activation of autophagy in these tissues. In contrast,the expression of these autophagy markers was signi?cantly decreased in OA synovium.Moreover,both Beclin-1and LC3were located mainly in the cells of the synovial lining layer and their expression patterns were the inverse of apoptotic markers[26,27].Therefore,autoph-agy is hyperactive in cells of the synovial lining in RA,and most of these are macrophages and RA-SFs,the major contributing factors to disease progression[30].
Very importantly,we showed that autophagy is inver-sely correlated with apoptosis in synovial tissues from OA and RA patients.In vitro,it was demonstrated that autophagy can limit ER stress response,which induces apoptosis when RA-and OA-SFs undergo Thapsigargin,a Ca2?–ATPase inhibitor,while transfection of Beclin-1 siRNA increased the susceptibility to ER stress-induced cell death[21].This evidence illustrated that the apoptosis of synovial cells in both OA and RA can be inhibited by autophagy.In consistence,we observed a higher autophagy while lower apoptosis in RA synovial lining layer cells.
MicroRNAs are involved in most cellular processes by inhibiting protein translation,destabilizing mRNA,or both. To explore the cause of enhanced autophagy,we checked miR-30a.There are miR-30a-binding sequences in the Beclin-130-UTR,and miR-30a was shown to inhibit Beclin-1expression[25].To explore the cause of enhanced autophagy in RA synovial tissues,we measured levels of miR-30a in both groups.Interestingly,we found that levels of miR-30a in the synovial tissues from RA patients were decreased in comparison to that of the OA.Furthermore, levels of Beclin-1mRNA decreased linearly with those of miR-30a.These data indicate that increased autophagy in RA synovial tissues probably results from the deregulation of miRA-30a.In support,previous studies demonstrated that miR-30a expression was downregulated via the pro-in?ammatory cytokines monocyte chemoattractant protein1 (MCP-1),RANTES,and IFN-inducible protein10(IP-10), all of which were signi?cantly increased in RA[32,33].Therefore,in?ammatory and immune abnormalities in RA may enhance autophagy,probably by downregulating miR-30a.
In summary,in the present study we demonstrated that apoptosis is decreased in synovial tissues from RA patients, compared with those from OA patients.By contrast,the higher expression of Beclin-1and LC3,and the presence of LC3-II,indicates upregulation of autophagy in RA,which may result from a de?ciency in miR-30a expression. Moreover,numbers of TUNEL-positive nuclei indicative of apoptosis were inversely correlated with autophagic markers.Thus,our data suggest that apoptotic resistance in synovial tissues from RA patients may be due to high levels of autophagy.
Acknowledgments We thank Jianbing Ma and Yumin Zhang for the collection of specimens.This study was supported by the National Natural Science Foundation of China(No.81171742)and Shaanxi Province Science and Technology Projects(No.2008K-38).
Con?ict of interest None.
References
1.Andersson AK,Li C,Brennan FM.Recent developments in the
immunobiology of rheumatoid arthritis.Arthritis Res Ther.
2008;10:204–12.
2.Humby F,Manzo A,Kirkham B,Pitzalis C.The synovial
membrane as a prognostic tool in rheumatoid arthritis.Autoim-mun Rev.2007;6:248–52.
3.Korb A,Pavenstadt H,Pap T.Cell death in rheumatoid arthritis.
Apoptosis.2009;14:447–54.
4.Wachsmann D,Sibilia J.Survival in the rheumatoid synovium.
Joint Bone Spine.2011;78:435–7.
5.Meinecke I,Cinski A,Baier A,Peters MA,Dankbar B,Wille A,
et al.Modi?cation of nuclear PML protein by SUMO-1regulates Fas-induced apoptosis in rheumatoid arthritis synovial?broblasts.
Proc Natl Acad Sci USA.2007;104:5073–8.
6.Perlman H,Liu H,Georganas C,Koch AE,Shamiyeh E,Haines
GK3rd,et al.Differential expression pattern of the antiapoptotic proteins,Bcl-2and FLIP,in experimental arthritis.Arthritis Rheum.2001;44:2899–908.
7.Bai SC,Liu HT,Chen KH,Eksarko P,Perlman H,Moore TL,et al.
NF-kappa B-regulated expression of cellular FLIP protects rheu-matoid arthritis synovial?broblasts from tumor necrosis factor alpha-mediated apoptosis.Arthritis Rheum.2004;50:3844–55. 8.Drynda A,Quax PHA,Neumann M,van der Laan WH,Pap G,
Drynda S,et al.Gene transfer of tissue inhibitor of metallopro-teinases-3reverses the inhibitory effects of TNF-alpha on fas-induced apoptosis in rheumatoid arthritis synovial?broblasts.
J Immunol.2005;174:6524–31.
9.Dharmapatni AASSK,Smith MD,Findlay DM,Holding CA,
Evdokiou A,Ahern MJ,et al.Elevated expression of caspase-3 inhibitors,survivin and xIAP correlates with low levels of apoptosis in active rheumatoid synovium.Arthritis Res Ther.
2009;11(1):R13.
10.Schwarten M,Mohrluder J,Ma PX,Stoldt M,Thielmann Y,Stangler
T,et al.Nix directly binds to GABARAP A possible crosstalk between apoptosis and autophagy.Autophagy.2009;5:690–8.
236K.Xu et al.
11.Eisenberg-Lerner A,Bialik S,Simon HU,Kimchi A.Life and
death partners:apoptosis,autophagy and the cross-talk between them.Cell Death Differ.2009;16:966–75.
12.Vellai T.Autophagy genes and ageing.Cell Death Differ.
2009;16:94–102.
13.Levine B,Kroemer G.Autophagy in the pathogenesis of disease.
Cell.2008;132:27–42.
14.Cecconi F,Levine B.The role of autophagy in mammalian
development:cell makeover rather than cell death.Dev Cell.
2008;15:344–57.
15.Sperandio S,de Belle I,Bredesen DE.An alternative,nonapop-
totic form of programmed cell death.Proc Natl Acad Sci USA.
2000;97:14376–81.
16.Kraft LJ,Kenworthy AK.Imaging protein complex formation in
the autophagy pathway:analysis of the interaction of LC3and Atg4B(C74A)in live cells using Forster resonance energy transfer and?uorescence recovery after photobleaching.J Bio-med Opt.2012;17:011008.
17.Vazquez CL,Colombo MI.Beclin1modulates the anti-apoptotic
activity of Bcl-2Insights from a pathogen infection system.
Autophagy.2010;6:177–8.
18.Furuya N,Yu F,By?eld M,Pattingre S,Levine B.The evolu-
tionarily conserved domain of Beclin1is required for Vps34 binding,autophagy and tumor suppressor function.Autophagy.
2005;1:46–52.
19.Kirkin V,McEwan DG,Novak I,Dikic I.A role for ubiquitin in
selective autophagy.Mol Cell.2009;34:259–69.
20.Kuma A,Matsui M,Mizushima N.LC3,an autophagosome
marker,can be incorporated into protein aggregates independent of autophagy.Autophagy.2007;3:323–8.
21.Shin YJ,Han SH,Kim DS,Lee GH,Yoo WH,Kang YM,et al.
Autophagy induction and CHOP under-expression promotes survival of?broblasts from rheumatoid arthritis patients under endoplasmic reticulum stress.Arthritis Res Ther.2010;12:R19.
22.Fassbender HG.Histomorphological basis of articular-cartilage
destruction in rheumatoid-arthritis.Coll Relat Res.1983;3:141–55.
23.MullerLadner U,Kriegsmann J,Franklin BN,Matsumoto S,
Geiler T,Gay RE,et al.Synovial?broblasts of patients with
rheumatoid arthritis attach to and invade normal human cartilage when engrafted into SCID mice.Am J Pathol.1996;149:1607–15.
24.Muller-Ladner U,Ospelt C,Gay S,Distler O,Pap T.Cells of the
synovium in rheumatoid arthritis—synovial?broblasts.Arthritis Res Ther.2007;9:223–32.
25.Zhu H,Wu H,Liu XP,Li BA,Chen Y,Ren XC,et al.Regulation
of autophagy by a beclin1-targeted microRNA,miR-30a,in cancer cells.Autophagy.2009;5:816–23.
26.Chen ZK,Wang LH.Expression of PDCD5gene in synovium of
rheumatoid arthritis.Chin J Rheumatol.2008;1:36–9.
27.Pap T,Franz JK,Hummel KM,Jeisy E,Gay R,Gay S.Activation
of synovial?broblasts in rheumatoid arthritis:lack of expression of the tumour suppressor PTEN at sites of invasive growth and destruction.Arthritis Res.2000;2:59–64.
28.Karantza-Wadsworth V,Patel S,Kravchuk O,Chen GH,Mathew R,
Jin S,et al.Autophagy mitigates metabolic stress and genome damage in mammary tumorigenesis.Genes Dev.2007;21:1621–35.
29.Mathew R,Kongara S,Beaudoin B,Karp CM,Bray K,Degen-
hardt K,et al.Autophagy suppresses tumor progression by limiting chromosomal instability.Genes Dev.2007;21:1367–81.
30.Smith MD,Weedon H,Papangelis V,Walker J,Roberts-Thom-
son PJ,Ahern MJ.Apoptosis in the rheumatoid arthritis synovial membrane:modulation by disease-modifying anti-rheumatic drug treatment.Rheumatology.2010;49:862–75.
31.Josefsen L,Droce A,Sondergaard TE,Sorensen JL,Bormann J,
Schafer W,et al.Autophagy provides nutrients for nonassimi-lating fungal structures and is necessary for plant colonization but not for infection in the necrotrophic plant pathogen Fusarium graminearum.Autophagy.2012;8:326–37.
32.Anglicheau D,Sharma VK,Ding RC,Hummel A,Snopkowski C,
Dadhania D,et al.MicroRNA expression pro?les predictive of human renal allograft status.Proc Natl Acad Sci USA.
2009;106(13):5330–5.
33.Kokkonen H,Soderstrom I,Rocklov J,Hallmans G,Lejon K,
Dahlqvist SR.Up-regulation of cytokines and chemokines predates the onset of rheumatoid arthritis.Arthritis Rheum.
2010;62(2):383–91.
Enhanced Autophagy in RA237
细胞凋亡试验常用的方法(MTT法、荧光法、DNA琼脂糖凝胶电泳法与流式细胞仪检测法) (一)药物对肿瘤细胞的抑制效应的MTT法: 用培养基将肿瘤细胞调整至2 X108个/L,在96孔板中每孔加入100ul细胞悬液于37℃、5% CO2下培养过夜。 次日每孔加入不同浓度的药物100mg/L作为试验组,设加完全培养基不加药物的阴性对照,并用功能明确的药物为阳性对照和0.5%的乙醇溶剂对照,每组均设4-6个复孔(平行孔)、37℃、5% CO2继续培养。 培养至12h、24h、48h、实验终止前4-6h加入10ulMTT(5g/L),培养4-6h后,阴性对照孔中已形成明显的蓝紫色颗粒结晶时加100ul/孔SDS-HCl终止反应,于37℃存放过夜。 用酶标仪在A570波长下测吸光度值,按下式计算抑制率 抑制率(%)=(1-试验组平均吸光度值/阴性对照组平均吸光度值)x 100%。 (二)荧光法: 选用上述最佳浓度作用于肿瘤细胞,培养细胞48h后,收货细胞用PBS洗2-3次后用0.4%多聚甲醛室温下固定30min。 弃去固定液,并用PBS洗2次后,用1%Triton X-100作用4min加入适量的0.5mg/L DAPI 荧光染色60min,用PBS冲洗3次,取10ul滴片,干燥后于荧光显微镜下检测断裂的颗粒和片状荧光。 (三)DNA琼脂糖凝胶电泳法: 1、DNA提取: 用大方瓶培养肿瘤细胞,每瓶10ml,细胞浓度为3 x 108个/ml,每隔药物浓度、作用时间均设2瓶,共分3个时间段,4个药物浓度。共培养26瓶细胞。 分别于细胞中加入不同浓度的药物,于37℃、5% CO2中分别培养12h、24h、48h,收货细胞,用PBS洗2-3次。 于-20℃将细胞冷却处理10min后将细胞收集至离心管中,加1ml细胞裂解液,再加蛋白酶K,轻轻振摇使悬液混匀,成黏糊状,50℃过夜。 冷却后加入等体积的饱和酚溶液,混合后10000r/min离心10min,吸出上层水相,移至另一离心管中,再加入等体积饱和酚溶液重复抽提一次,直到无蛋白为止。 吸上清加入氯仿/异戊醇(24:1)按上述方法再抽提一次。 吸取水相层加入1/10体积的3mol/L的醋酸钠溶液,混匀。 再加入2.5倍体积冷无水乙醇,混合置-20℃处理30min后,10000r/min离心10min,沉淀部分为提供的DNA,弃去无水乙醇后用70%乙醇漂洗2次,将离心管倒扣在吸水纸上,吸干乙醇。 加入200ulTE缓冲液融解DNA,再加入25ul的RNA酶,置37℃作用30min,置4℃冰箱保存。 2、琼脂糖凝胶电泳: TBE缓冲液配制1.8%琼脂糖凝胶。在微波炉内煮沸至琼脂糖融解,待冷却至60℃时,加入溴化乙锭,使其终浓度为0.5mg/ml,混匀后灌胶。 待凝胶固定后放入含TBE电泳液的电泳槽内,使TBE电泳液盖过凝胶。 取10-15ul提取的各组DNA样品液与上样缓冲液按4:1比例混匀后点样。 60V电泳1h,用紫外透射仪观察梯形条带。
实验目的: 1.了解凋亡细胞的形态学特征,加深对于细胞凋亡现象及本质的理解。 2.了解并掌握细胞凋亡检测的方法和基本原理。 实验原理: 细胞凋亡时,出现一系列形态学变化,包括凋亡细胞的染色质浓缩、边缘化,核膜裂解、染色质分割成块状,染色质的DNA出现缺口甚至断裂,出现DNA碎片,并逐渐形成凋亡小体等,经相应的染色后可以在普通光学显微镜和荧光显微镜下观察到这些变化。从而把凋亡的细胞和正常的细胞区分开来。
细胞凋亡是指细胞对环境的生理、病理性刺激信号、环境条件的变化或缓和性损伤产生的应答有序变化的死亡过程。细胞凋亡是一个主动过程,涉及一系列基因的激活、表达以及调控等的作用,它并不是病理条件下的自体损伤,而是为更好地适应生存环境的一种死亡过程。 1.细胞凋亡与细胞程序性死亡: 细胞程序性死亡的概念是指一个多细胞生物体中某些细胞的死亡是个体发育中一个预定的,并受到严格程序控制的正常组成部分。例如蝌蚪变成青蛙,其变态过程中尾部的消失伴随大量细胞死亡,高等哺乳类动物指间蹼的消失、颚融合、视网膜发育以及免疫系统的正常发育都必须有细胞死亡的参与。这些形形色色的在机体发育过程中出现的细胞死亡有一个共同特征:即散在的、逐个地从正常组织中死亡和消失,机体没有炎症反应,而且这种死亡对整个机体的发育是有利和必须的。因此认为动物发育过程中存在的细胞程序性死亡是一个发育学概念,而细胞凋亡则是一个形态学的概念,但是一般认为这两个概念可以交互使用,具有同等意义。2.细胞凋亡与坏死的区别: 虽然凋亡与坏死的最终结果极为相似,但它们的过程与表现却有很大差别。坏死是细胞受到强烈理化或生物因素作用引起细胞无序变化的死亡过程。表现为细胞胀大、胞膜破裂、细胞内容物外溢、核变化较慢、DNA降解不充分、有局部严重的炎症反应。坏死是一个被动的过程,其细胞及组织的变化与凋亡有明显的不同。
题目:秀丽线虫生殖细胞凋亡检测 实验目的: 1. 掌握检测凋亡细胞的方法 2. 学习使用荧光染料活体染色的方法和步骤 .实验原理 1. 秀丽隐杆线虫( Caenorhabditis elegans ):是一种无毒无害、可以独立生存的 线虫。其个体小,成体仅 1.5mm 长,为雌雄同体 ( hermaphrodites ),雄性个体仅占群体的 0.2%,可自体受精或双性生殖;在20℃下平均生活史为 3.5 天,平均繁殖力为 300-350 个;但若与雄虫交配,可产生多达 1400 个以上的后代。 1976 年, Sulston 和 Horvitz 利用秀丽隐杆线虫 ( Caenorhabditis elegans ) 研究发现,其约 13%的体细胞在胚胎发育中注定死亡,使得人们认识到细胞凋亡的遗传基础。 2. 荧光染料活体染色:本实验使用吖啶橙( Acridine orange )作为染色剂,该染 料对细胞具有慢性毒性,致癌性强,由于凋亡细胞因 DNA片段化可结合更多染料,荧光显微镜下呈亮绿色,可在荧光显微镜下快速方便的检测出,适用于多数品系。
实验材料及设备 1. 实验材料: a) 各品系秀丽隐杆线虫:N2(实验组) , ced-1::gfp (方法对照组),ced- 3(阴性对照) b) OP50 c) M9培养基 d) NGM培养基 2. 实验设备: a) 普通光学显微镜 b) 载玻片若干,盖玻片若干,铂金丝 c) 暗箱 d) 吸水纸、滴管等 e) 荧光显微镜 四.实验方法及步骤 1. 线虫接种、同步化 2. 取样:在 12 孔板培养板上,每孔吸取 900μL 预先接入少量 OP50 的 M9 培养基,每孔用铂金丝挑取培养 20~30 条成体线虫 3. 染色:向 N2与 ced-3 品系中每孔加入 250μg/mL 吖啶橙 100μL, 混匀后 置于培养箱(避光)染色 45~60min。 4. 方法对照组观察:向 ced-1::GFP 品系中加入 1 滴盐酸左旋咪唑,麻痹线
细胞凋亡检测方法 一、细胞凋亡的形态学检测 1 光学显微镜和倒置显微镜 (1)未染色细胞:凋亡细胞的体积变小、变形,全面皱缩,细胞膜完整但出现发泡现象,细胞凋亡晚期可见凋亡小体,凋亡小体为数个圆形小体围绕在细胞周围。贴壁细胞出现皱缩、变圆、脱落。 (2)染色细胞: 姬姆萨(Giemsa)染色、瑞氏染色等:正常细胞核色泽均一;凋亡细胞染色质浓缩、边缘化,核膜裂解、染色质分割成块状和凋亡小体等典型的凋亡形态;坏死细胞染色浅或没染上颜色。 苏木素-伊红(HE)染色:细胞核固缩碎裂、呈蓝黑色、胞浆呈淡红色(凋亡细胞),正常细胞核呈均匀淡蓝色或蓝色,坏死细胞核呈很淡的蓝色或蓝色消失。 2 荧光显微镜和共聚焦激光扫描显微镜 一般以细胞核染色质的形态学改变为指标来评判细胞凋亡的进展情况。 常用的DNA特异性染料有:Hoechst 33342,Hoechst 33258,DAPI。三种染料与DNA 的结合是非嵌入式的,主要结合在DNA的A-T碱基区。紫外光激发时发射明亮的蓝色荧光。 Hoechst是与DNA特异结合的活性染料,能进入正常细胞膜而对细胞没有太大细胞毒作用。Hoechst 33342在凋亡细胞中的荧光强度要比正常细胞中要高。 DAPI为半通透性,用于常规固定细胞的染色。 PI和Hoechst33342双标:PI、Hoechst33342均可与细胞核DNA(或RNA)结合。但PI不能通过正常细胞膜,Hoechst则为膜通透性荧光染料,故细胞在处于坏死或晚期调
亡时细胞膜被破坏,这时可为PI着红色。正常细胞和中早期调亡细胞均可被Hoechst着色,但是正常细胞核的Hoechst着色的形态呈圆形,淡兰色,内有较深的兰色颗粒;而调亡细胞的核由于浓集而呈亮兰色,或核呈分叶,碎片状,边集。故PI着色为坏死细胞;亮兰色,或核呈分叶状,边集的Hoechst着色的为调亡细胞。 凋亡细胞体积变小,细胞质浓缩。细胞凋亡过程中细胞核染色质的形态学改变分为三期:Ⅰ期的细胞核呈波纹状(rippled)或呈折缝样(creased),部分染色质出现浓缩状态;Ⅱa期细胞核的染色质高度凝聚、边缘化;Ⅱb期的细胞核裂解为碎块,产生凋亡小体(图1)。 3 透射电子显微镜观察 凋亡细胞体积变小,细胞质浓缩。凋亡Ⅰ期(pro-apoptosis nuclei)的细胞核内染色质高度盘绕,出现许多称为气穴现象(cavitations)的空泡结构(图2);Ⅱa期细胞核的染色质高度凝聚、边缘化;细胞凋亡的晚期,细胞核裂解为碎块,产生凋亡小体。 二、磷脂酰丝氨酸外翻分析(Annexin V法) 磷脂酰丝氨酸(Phosphatidylserine, PS)正常位于细胞膜内侧,但在细胞凋亡早期,PS可从细胞膜内侧翻转到细胞膜表面,暴露在细胞外环境中。磷脂酰丝氨酸的转位发生在凋亡早期阶段,先于细胞核的改变、DNA断裂、细胞膜起泡。体内的吞噬细胞可通过识别
细胞凋亡实验步骤及注意事项 一、实验目的 1、掌屋凋亡细胞的形态特征 2、学会用荧光探针对细胞进行双标记来检测正常活细胞、凋亡细胞与坏死 细胞的方法 二、实验原理 细胞死亡根据其性质、起源及生物学意义区分为凋亡与坏死两种不同类型。凋亡普遍存在于生命界,在生物个体与生存中起着非常重要的作用。它就是细胞在一 定生理条件下一系列顺序发生事件的组合,就是细胞遵循一定规律自己结束生命 的自主控制过程。细胞凋亡具有可鉴别的形态学与生物化学特征。 在形态上可见凋亡细胞与周围细胞脱离接触,细胞变园,细胞膜向内皱缩、胞浆浓缩、内质网扩张、细胞核固缩破裂呈团块状或新月状分布、内质网与细胞膜进一步融合将细胞分成多个完整包裹的凋亡小体,凋亡小体最后被吞噬细胞吞噬消化。在凋亡过程中细胞内容物并不释放到细胞外,不会影响其它细胞,因而不引起炎症反应。 在生物化学上,多数细胞凋亡的过程中,内源性核酸内切酶活化,活性增加。核DNA 随机地在核小体的连接部位被酶切断,降解为180-200bp或它的整倍数的各种片断。如果对核DNA进行琼脂糖电泳,可显示以180-200bp为基数的DNA ladder(梯状带纹)的特征。 相比之下,坏死就是细胞处于剧烈损伤条件下发生的细胞死亡。细胞在坏死早期 即丧失质膜完整性,各种细胞器膨胀,进而质膜崩解释放出其中的内容物,引起炎症反应,坏死过程中细胞核DNA虽也降解,但由于存在各种长度不等的DNA片断,不能形成梯状带纹,而呈弥散状。 一些温与的损伤刺激及一些抗肿瘤药物可诱导细胞凋亡,通常这些因素在诱导凋亡的同时,也可产生细胞坏死,这取决于损伤的剧烈程度与细胞本身对刺激的敏感 程度。 三尖杉酯碱(HT)就是我国自行研制的一种对急性粒细胞白血病,急性单核白血病等有良好疗效的抗肿瘤药物。研究表明HT在0、02~5μg/ml范围内作用2小时,即可诱导HL-60细胞凋亡,并表现出典型的凋亡特征。本实验用1μg/ml HT在体外诱导培养的HL-60细胞发生凋亡,同时也有少数细胞发生坏死。用 Hoechst33342与碘化丙啶(propidium iodide,PI)对细胞进行双重染色,可以区别凋亡、坏死及正常细胞。 细胞膜就是一选择性的生物膜,一般的生物染料如PI等不能穿过质膜。当细胞坏死时,质膜不完整,PI就进入细胞内部,它可嵌入到DNA或RNA中,使坏死细胞着
细胞生物学实验报告 淋巴细胞分离和细胞凋亡诱导及形态学观察lymphocyte isolation and morphological observation of apoptosis induction 2012年6月2日
淋巴细胞分离和细胞凋亡诱导及形态学观察 lymphocyte isolation and morphological observation of apoptosis induction 摘要:目的了解细胞凋亡的原理,掌握离体诱导细胞凋亡的方法,及用普通光学显微镜和荧光显微镜观察凋亡细胞的形态学变化,并从观察结果初步推断和识别凋亡细胞具体阶段。方法实验所用Hoechst 33342/PI双染检测细胞凋亡、Giemsa染色。结果实验结束后得到了染色的结果以及照片。结论所提取的淋巴细胞发生凋亡。 Abstract:Objective Understand the principles of cell apoptosis, master the methods of cell apoptosis induced by in vitro, and by ordinary optical microscopy and fluorescence microscopy observation of morphological changes of apoptotic cells and preliminary inferred from observations and identifying apoptotic cells specific stages. Method Experimental method used in,Hoechst 33342/PI double dye test and the Giemsa stain. Results Be dyed after the end of the experiment results and photos. Conclusions The extraction of lymphocyte apoptosis. 关键词:细胞凋亡、Giemsa染色、Hoechst 33342/PI双染。 Keyword:cell apoptosis、Giemsa stain、Hoechst 33342/PI double staining 1.实验原理 1.1 关于淋巴细胞的分离 外周血中淋巴细胞比重约为1.070,而红细胞和粒细胞的比重较大,为1.902左右。因此,利用相对密度为1.077±0.002的淋巴细胞分离液(称为分层液)离心,可使一定比重的细胞按相应密度梯度分布(使比重中较大的红细胞和粒细胞沉于管底,淋巴细胞浮于分层液与血浆的界面上),从而将淋巴细胞分离出来。 1.2 关于细胞凋亡 细胞凋亡又称编程性死亡或程序性死亡。细胞凋亡是多细胞生物体在发育过程中或在某些环境因子的作用下发生的受基因调控的主动的死亡方式。细胞凋亡对于多细胞生物个体的正常发育、保持自稳平衡、抵御外界各种因素的干扰及多种病理过程具有极其重要的意义,起着非常重要的作用。细胞凋亡是多种生理、病理因子参与的由凋亡相关基因启动的细胞程序性死亡过程,其中由氧应激造成大量活性氧(reactive oxygen species, ROS)的产生以及继发性细胞损伤过程在细胞凋亡中起着重要作用,如电离辐射或紫外线照射产生大量H2O2、OH-等。 细胞凋亡的诱导因子包括三大类: 1.物理因子:包括射线、较温和的温度刺激(如热激或冷激)等; 2.化学因子:包括活性氧基团和分子、重金属离子等; 3.生物因子:肿瘤坏死因子、生物毒素、抗肿瘤药物、DNA和蛋白质合成的抑制剂等。 细胞凋亡的主要特征包括: 1.染色质凝集、质膜出芽、核裂解及凋亡小体的形成。 2.DNA特异性降解成200bp或其整数倍片断,通过凝胶电泳形成梯状条带,称为DNA Ladder。 3.由于DNA特异性降解而产生大量3’-OH末端,可被末端脱氧核糖核苷酸移换酶介导的dUTP 缺口末端原位标记法(TUNEL)标记,从而产生亮绿色荧光等。
实验14 细胞凋亡的诱导和检测 20世纪60年代人们注意到细胞存在着两种不同形式的死亡方式:凋亡(apoptosis)和坏死(necrosis)。细胞坏死指病理情况下细胞的意外死亡,坏死过程细胞膜通透性增高,细胞肿胀,核碎裂,继而溶酶体、细胞膜破坏,细胞容物溢出,细胞坏死常引起炎症反应。 细胞凋亡apoptosis一词来源于古希腊语,意思是花瓣或树叶凋落,意味着生命走到了尽头,细胞到了一定时期会像树叶那样自然死亡。凋亡是细胞在一定生理或病理条件下遵守自身程序的主动死亡过程。凋亡时细胞皱缩,表面微绒毛消失,染色质凝集并呈新月形或块状靠近核膜边缘,继而核裂解,由细胞膜包裹着核碎片或其他细胞器形成小球状凋亡小体凸出于细胞表面,最后凋亡小体脱落被吞噬细胞或邻周细胞吞噬。凋亡过程中溶酶体及细胞膜保持完整,不引起炎症反应。细胞凋亡时的生化变化特征是核酸切酶被激活,染色体DNA被降解,断裂为50~300 kb长的DNA片段,再进一步断裂成180~200bp整倍数的寡核苷酸片断,在琼脂糖凝胶电泳上呈现“梯状”电泳图谱(DNA Ladder)。细胞凋亡在个体正常发育、紫稳态维持、免疫耐受形成、肿瘤监控和抵御各种外界因素干扰等方面都起着关键性的作用。 1.细胞凋亡的检测方法 凋亡细胞具有一些列不同于坏死细胞的形态特征和生化特征,据此可以鉴别细胞的死亡形式。细胞凋亡的机制十分复杂,一般采用多种方法综合加以判断,同时不同类型细胞的凋亡分析方法有所不同,方法选择依赖于具体的研究体系和研究目的(表?)。
形态学观察方法:利用各种染色法可观察到凋亡细胞的各种形态学特征: (1)DAPI时常用的一种与DNA结合的荧光染料。借助于DAPI染色,可以观察细胞核的形态变化。 (2)Giemsa染色法可以观察到染色质固缩、趋边、凋亡小体形成等形态。 (3)吖啶橙(AO)染色,荧光显微镜观察,活细胞核呈黄绿色荧光,胞质呈红色荧光。凋亡细胞核染色质呈黄绿色浓聚在核膜侧,可见细胞膜呈泡状膨出及凋亡小体。 (4)吖啶橙(A())/溴化乙啶(EB)复染可以更可靠地确定凋亡细胞的变化,AO只进入活细胞,正常细胞及处于凋亡早期的细胞核呈现绿色;EB只进入死细胞,将死细胞及凋亡晚期的细胞的核染成橙红色。 (5)台盼蓝染色对反映细胞膜的完整性,区别坏死细胞有一定的帮助,如果细胞膜不完整、破裂,台盼蓝染料进入细胞,细胞变蓝,即为坏死。如果细胞膜完整,细胞不为台盼蓝染色,则为正常细胞或凋亡细胞。使用透射电镜观察,可见凋亡细胞表面微绒毛消失,核染色质固缩、边集,常呈新月形,核膜皱褶,胞质紧实,细胞器集中,胞膜起泡或出“芽”及凋亡小体和凋亡小体被临近巨噬细胞吞噬现象。 (6)木精-伊红(HE)染色是经典的显示细胞核、细胞质的染色方法,染色结果清晰。发生凋亡的细胞经HE染色后,其细胞大小的变化及特征性细胞核的变化:染色质凝集、呈新月形或块状靠近核膜边缘,晚期核裂解、细胞膜包裹着核碎片“出芽”凸出于细胞表面形成凋亡小体等均可明显显示出来。 DNA凝胶电泳:细胞发生凋亡或坏死,其细胞DNA均发生断裂,细胞小分子 质量DNA片段增加,高分子DNA减少,胞质出现DNA片段。但凋亡细胞DNA断裂点均有规律的发生在核小体之间,出现180~200 bp DNA片段,而坏死细胞的DNA断裂点为无特征的杂乱片段,利用此特征可以确定群体细胞的死亡,并可与坏死细胞区别。
常用细胞凋亡检测方法(图) 转载请注明来自丁香园 发布日期:2012-02-16 13:41 文章来源:丁香通 关键词:丁香园生物专题义翘神州细胞培养点击次数:951 一、细胞凋亡的形态学检测 1、光学显微镜和倒置显微镜 ①未染色细胞:凋亡细胞的体积变小、变形,细胞膜完整但出现发泡现象,细胞凋亡晚期可见凋亡小体。贴壁细胞出现皱缩、变圆、脱落。 ②染色细胞:常用姬姆萨染色、瑞氏染色等。凋亡细胞的染色质浓缩、边缘化,核膜裂解、染色质分割成块状和凋亡小体等典型的凋亡形态。 2、荧光显微镜和共聚焦激光扫描显微镜 一般以细胞核染色质的形态学改变为指标来评判细胞凋亡的进展情况。常用的DNA 特异性染料有:HO 33342 (Hoechst 33342),HO 33258 (Hoechst 33258), DAPI。三种种染料与DNA的结合是非嵌入式的,主要结合在DNA的A-T碱基区。紫外光激发时发射明亮的蓝色荧光。Hoechst是与DNA特异结合的活性染料,储存液用蒸馏水配成1mg/ml的浓度,使用时用PBS稀释,终浓度为10 ug/ml。DAPI为半通透性,用于常规固定细胞的染色。储存液用蒸馏水配成1mg/ml的浓度,使用终浓度一般为10 ug/ml。结果评判:细胞凋亡过程中细胞核染色质的形态学改变分为三期:Ⅰ期的细胞核呈波纹状(rippled)或呈折缝样(creased),部分染色质出现浓缩状态;Ⅱa期细胞核的染色质高度凝聚、边缘化;Ⅱb期的细胞核裂解为碎块,产生凋亡小体(图1)。 3、透射电子显微镜观察 结果评判:凋亡细胞体积变小,细胞质浓缩。凋亡Ⅰ期(pro-apoptosis nuclei)的细胞核内染色质高度盘绕,出现许多称为气穴现象(cavitations)的空泡结构(图2);Ⅱa期细胞核的染色质高度凝聚、边缘化;细胞凋亡的晚期,细胞核裂解为碎块,产生凋亡小体。 二、磷脂酰丝氨酸外翻分析(Annexin V法) 磷脂酰丝氨酸(Phosphatidylserine, PS)正常位于细胞膜的内侧,但在细胞凋亡的早期,PS可从细胞膜的内侧翻转到细胞膜的表面,暴露在细胞外环境中(图3)。Annexin-V是一种分子量为35~36KD的Ca2+依赖性磷脂结合蛋白,能与PS高亲和力特异性结合。将Annexin-V进行荧光素(FITC、PE)或biotin标记,以标记了的Annexin-V作为荧光探针,利用流式细胞仪或荧光显微镜可检测细胞凋亡的发生。 碘化丙啶(propidine iodide, PI)是一种核酸染料,它不能透过完整的细胞膜,但在凋亡中晚期的细胞和死细胞,PI能够透过细胞膜而使细核红染。因此将Annexin-V 与PI匹配使用,就可以将凋亡早晚期的细胞以及死细胞区分开来。 方法
细胞凋亡实验技术总结 一形态学检测 1、光学显微镜和倒置显微镜观察法 未染色细胞:凋亡细胞体积变小、变形,膜完整但出现发泡现象,晚期出现凋亡小体。贴壁细胞出现皱缩,变圆,脱落。染色细胞:姬姆萨染色,瑞氏染色等。凋亡细胞染色质浓缩,边缘化,核膜裂解,染色质分割成块状,形成凋亡小体。 2、荧光显微镜检测法-荧光染料 例如,碘化丙啶(PI)是一种核酸染料,它不能透过完整的细胞膜,但在凋亡中晚期的细胞和死细胞,PI 能够透过细胞膜而使细胞核红染。选用536nm 激发光,细胞核呈红色荧光。 3、电子显微镜 收集细胞,2.5%戊二醛4°C 固定24h,1%四氧化锇后固定,丙酮梯度脱水,经包埋剂浸透后环氧树脂包埋,超薄切片,醋酸铀和枸橼酸铅双重染色,透射电镜观察。凋亡Ⅰ期的细胞核内染色质高度盘绕,出现许多称为气穴现象的空泡结构。Ⅱa 期细胞核的染色质高度凝聚、边缘化;细胞凋亡的晚期,细胞核裂解为碎块,产生凋亡小体。 4、激光扫描共焦显微镜技术 FITC-AnnexinV+PI双染,观察凋亡过程中细胞膜PS表面的变化,并区分正常细胞(An-PI-),早期凋亡细胞(An+PI-),晚期凋亡细胞及坏死细胞(An+PI+),细胞收集过程中出现的损伤细胞(An-PI+)。 二、细胞凋亡的生化及分子生物学检测 1、DNA 断裂检测法 如使用琼脂糖凝胶电泳检测,细胞凋亡时,核染色质凝聚,染色质DNA 在核小体单位之间的连接处断裂。凋亡早期可形成50~300kbp 的DNA 大片段,晚期核酸内切酶在核小体之间剪切核DNA,产生大量长度在180~200bp 整数倍的寡核苷酸片段。 2、膜联蛋白V 法 磷脂酰丝氨酸(PS)位于正常细胞膜的内侧,但在细胞凋亡的早期,PS 可从细胞膜的内侧翻转到细胞膜表面。Annexin-Ⅴ(膜联蛋白-V)是一种分子量为35-36KD 的Ca2+ 依赖性磷脂结合蛋白,与PS高亲和力。将Annexin-Ⅴ进行荧光素或生物素标记,以标记了的Annexin-Ⅴ作为探针,利用流式细胞仪、荧光显微镜以及共聚焦激光扫描显微镜检测细胞凋亡的发生。 3、细胞凋亡的酶Caspase检测 检测Caspase活力可用免疫杂交技术分析酶原的加工和底物水解的产物,或用人工底物检测酶活力,也可对活化的Caspase做亲和标记。例如分析底物的水解产物,PARP(多聚ADP-核糖聚合酶)第一个被认识的caspase-3底物,它的相对分子质量为116000,水解后形成相对分子质量为85000 及相对分子质量为25000 的两个片段,用抗相对分子质量为85000 片段的抗体检测细胞是否发生凋亡。 4、线粒体膜势能变化的检测 线粒体跨膜电位的存在,使一些亲脂性阳离子荧光染料可结合到线粒体基质,其荧光的增强或减弱反映了线粒体内膜电负性的增高或降低流式细胞仪检测细胞的荧光强度或荧光显微镜观察,拍照正常细胞中, Rh123 能够依赖线粒体跨膜电位进入线粒体基质,荧光强度减弱或消失。而凋亡时,线粒体膜完整性破坏,线粒体膜通透性转运孔开放,引起线粒体跨膜电位的崩溃, Rh123 重新释放出线粒体, 从而发出强黄绿色荧光。
实验七、Hela细胞凋亡诱导及检测 一、实验目的 学习细胞凋亡诱导及检测。 二、实验原理 1.细胞凋亡是多细胞有机体为调控机体发育,维护内环境稳定,由基因控制的细 胞主动死亡过程,是细胞衰老自然死亡的主要方式之一,是一种自然的生理学 过程。与细胞坏死不同,不会引起炎症反应,不释放细胞内容物。 2.DAPI是一种荧光染料,它可以与DNA双螺旋的凹槽部分发生相互作用,从而与 DNA紧密结合,可在紫外下激发蓝光。 三、实验材料 8.8mol/L的H2O2溶液,甲醇,PBS溶液,10μg/mL的DAPI染液 四、实验步骤 1.细胞传代(上一次实验完成) 2.凋亡诱导 1)取做H.E染色的小皿,加H2O2溶液150μL使终浓度为0.8mol/L 2)24小时后收集细胞进行染色和形态学观察。 3. 染色 1)收集细胞,观察,贴壁细胞较多,直接用PBS溶液洗 2)吸出洗液,加入500μL甲醇,室温固定10min 3)倒掉甲醇,PBS洗净,加500μLPBS溶液和50μLDAPI母液,于37℃染色10min 4)倒掉染液,用PBS洗净(注意避光),加入500μLPBS溶液,倒置荧光显微镜 下观察并拍照。 五、实验结果与分析 1.观察: 实验开始前镜检: 细胞贴壁较多,细胞有的仍呈不规则状,有的细胞已皱缩,还有一些细胞呈圆形浮在培养基中,核质分界不明显。可以看到有的细胞处于裂解状态。 染色后: 由于DAPI染料只对核进行染色,所以在紫外下只可见核的结构。 视野里最多的是正常细胞,其特点是染色质均一且核表面光滑,说明凋亡是不同步的。 凋亡各时期的细胞也都可见,其主要特点是染色不均一。凋亡前期和中期的细胞较多。很少看到凋亡末期的细胞,除了这个时期细胞较少外,还可能因 为在前期操作中很多凋亡小体被洗掉了。而且有的细胞在正常光下观察是明显 的裂解状态,但是到紫外光路下就变得很不明显了。 另外,可以看到很多分裂期的细胞,其特点为染色深,细胞核染色质浓缩,但是看起来较均一,往往有对称性,特别是分裂末期的细胞两个子细胞会靠在 一起。 2.照片及分析:
细胞凋亡的几种检测方法 1、形态学观察方法 (1)HE(苏木精—伊红染色法)染色、光镜观察:凋亡细胞呈圆形,胞核深染,胞质浓缩,染色质成团块状,细胞表面有“出芽”现象。 (2)丫啶橙(AO)染色,荧光显微镜观察:活细胞核呈黄绿色荧光,胞质呈红色荧光。凋亡细胞核染色质呈黄绿色浓聚在核膜内侧,可见细胞膜呈泡状膨出及凋亡小体。 (3)台盼蓝染色:如果细胞膜不完整、破裂,台盼蓝染料进入细胞,细胞变蓝,即为坏死。如果细胞膜完整,细胞不为台盼蓝染色,则为正常细胞或凋亡细胞。此方法对反映细胞膜的完整性,区别坏死细胞有一定的帮助。 (4)透射电镜观察:可见凋亡细胞表面微绒毛消失,核染色质固缩、边集,常呈新月形,核膜皱褶,胞质紧实,细胞器集中,胞膜起泡或出“芽”及凋亡小体和凋亡小体被临近巨噬细胞吞噬现象。 2、DNA凝胶电泳 细胞发生凋亡或坏死,其细胞DNA均发生断裂,细胞内小分子量DNA片断增加,高分子DNA减少,胞质内出现DNA片断。但凋亡细胞DNA断裂点均有规律的发
生在核小体之间,出现180-200bpDNA片断,而坏死细胞的DNA断裂点为无特征的杂乱片断,利用此特征可以确定群体细胞的死亡,并可与坏死细胞区别。正常活细胞DNA 电泳出现阶梯状(LADDER)条带;坏死细胞DNA电泳类似血抹片时的连续性条带 3、酶联免疫吸附法(ELISA)核小体测定 凋亡细胞的DNA断裂使细胞质内出现核小体。核小体由组蛋白及其伴随的DNA片断组成,可由ELISA法检测。 检测步骤 1、将凋亡细胞裂解后高速离心,其上清液中含有核小体; 2、在微定量板上吸附组蛋白体’ 3、加上清夜使抗组蛋白抗体与核小体上的组蛋白结合‘ 4、加辣过氧化物酶标记的抗DNA抗体使之与核小体上的DNA结合’ 4、加酶的底物,测光吸收制。 用途 该法敏感性高,可检测5*100/ml个凋亡细胞。可用于人、大鼠、小鼠的凋亡检测。该法不需要特殊仪器,
细胞在发生凋亡时,会激活一些DNA内切酶,这些内切酶会切断核小体间的基因组DNA。基因组DNA 断裂时,暴露的3'-0H 可以在末端脱氧核苷酸转移酶(Terminal Deox yn ucleotidyl Tran sferase,TdT)的催化下加上荧光素(FITC)标记的dUTP(fluorescein-dUTP),从而可以通过荧光显微镜或流式细胞仪进行检测,这就是TUNEL 法检测细胞凋亡的原理。 TUNEL法特异性检测细胞凋亡时产生的DNA断裂,但不会检测出射线等诱导的DNA断裂(和细胞凋亡时的断裂方式不同)。这样一方面可以把凋亡和坏死区分开,另一方面也不会把 射线等诱导发生DNA断裂的非凋亡细胞判断为凋亡细胞。 针对问题2(TUNEL法的实验原理是什么?): 基本原理:对不同组织切片先增加细胞膜通透性,然后让rTDT和bio标记的dUTP进入细 胞内,在rTDT的辅助下dUTP与核断裂的DNA 3 -0H结合,再用HRP标记的链霉亲和素与dUTP 上的biot in 结合(每个链霉亲和素至少可以再结合3个biot in 分子),最后用DAB 过氧化氢与SP上的辣根过氧化物酶HRP发生氧化、环化反应,形成苯乙肼聚合物而呈现棕褐色,最终通过计数每张切片上不同视野中TUNEL阳性细胞的比例来判断细胞凋亡发生情 况。■ 1. TUNEL工作原理:简单说就是一一TUNEL细胞凋亡检测试剂盒是用来检测细胞在凋亡过程中细胞核DNA的断裂情况。 其原理是;生物素(biot in )标记的dUTP在脱氧核糖核苷酸末端转移酶(TdT En zyme)的 作用下,可以连接到凋亡细胞中断裂的DNA的3' - 0H末端,并可与连接了的辣根过氧化酶的 链霉亲和素(Streptavidin-HRP )特异结合,在辣根过氧化酶底物二氨基联苯胺(DAB的存在下,产生很强的颜色反应(呈深棕色),特异准确地定位正在凋亡的细胞,因而在普通 显微镜下即可观察和计数凋亡细胞;由于正常的或正在增殖的细胞几乎没有DNA的断裂,因而没有3'-0H形成,很少能够被染色。 针对问题3 (TUNEL实验中几个关键步骤是什么?): 1. 充分脱蜡和水化。脱蜡可以先60度20min,再用二甲苯两次5~10min ;而水化用梯度乙 醇从高浓度到低浓度浸洗,这些以便后面的结合反应充分、均匀; 2. 把握好细胞通透的时间。一般根据切片的厚薄,选择蛋白酶k的孵育时间,常用10~30min, 几um切片用短时间;几十um切片用长时间,通过摸索达到既不脱片,有能够使后面的酶和 抗体进入胞内。 3. 适当延长TUNEL反应液的时间。一般是37度1h,你也可以根据你的凋亡损伤程度,选择更长的时间,可长至2h,但要结合你最终的背景着色。 4. DAB显色条件的选择。一般DAB反应10分钟左右,结合镜下控制背景颜色,最长不超过 30min;我不喜欢用promega公司提供的DAB液(桃红色),不利于辨认棕褐色。 5. PBS的充分清洗。我个人认为,在TUNEL反应后和酶标反应后的清洗应十分严格,可增加 次数达5次,因为这些清洗直接决定最后切片的非特异性着色。 6. 此外,内源性POD的封闭也十分关键。对于肝脏、肾脏等血细胞含量多的组织,我的经 验是适当延长封闭时间和升高过氧化氢的浓度,可以达到很好的封闭效果,且不影响最终的 特异性染色。 针对问题5.细胞通透的原理、通透剂的浓度、孵育时间及其配制方法? 1. 蛋白酶K是消化膜蛋白,从而起打孔作用,增加
细胞凋亡 同学们好,这一讲开始我们来学习细胞凋亡的检测方法。 细胞死亡的方式有很多种,最常见的有坏死(necrosis),它是细胞受到物理或化学损伤的情况下,以及缺氧时会发生的现象,另一种常见的死亡方式是细胞凋亡(apoptosis),又称细胞程序性死亡,它是细胞主动的有序的死亡过程,用来去除多余的,不需要的或异常的细胞,保障生物体内环境的稳定,是一种基本的生物学现象。其他死亡方式还有自噬性细胞死亡(autophagic cell death)和细胞焦亡(Pyroptosis)。随着生命科学的发展,这些死亡方式逐渐进入我们的视野,被关注。 不同的死亡方式有着各自的特征。比如坏死,从形态学上观察,胞体肿胀、胞质空泡化,胞膜破损、最后崩解,所以坏死又称细胞胀亡(Oncosis)。而细胞凋亡,胞体缩小,膜表面出芽状形成凋亡小体,最终从细胞表面脱落,膜基本保持完整、。 细胞凋亡研究有着非常重要的生理和病理意义,2002年诺贝尔生理学或医学奖就授予了细胞程序性死亡方面的研究工作。细胞凋亡参与机体的正常发育与分化、内环境的稳定、免疫系统防御等重要的生理过程,一旦凋亡异常就会导致一些重大疾病的发生与发展,比如肿瘤的发生,肿瘤早期阶段细胞凋亡都是受到抑制的,诱导肿瘤细胞凋亡已成为抗肿瘤药物研发的一个重要方向。 近年来,许多细胞凋亡检测方法得到广泛的应用。下面介绍四种近年来细胞凋亡的主要检测方法: 一、形态学观察 细胞发生凋亡时会出现一系列独特的形态学特征,如细胞体积变小;核固缩,染色质高度凝聚,且堆积在核膜内侧缘或聚集于核中央部;接着凋亡小体的产生,细胞膜皱褶、细胞表面产生了许多泡状或芽状突起,形成单个的凋亡小体。借用光学显微镜、电子显微镜或荧光显微镜可不同程度、不同层次地观测到这些形态学特征。这种细胞凋亡形态学检测的方法简易、直观和有较好定位,但也有不足之处:缺乏特定标准,主观性大,因人而异;又不能定量,有较大的局限性,因而形态学观察多用于固定组织细胞检测,常作为其他技术的辅助。 二、流式细胞术 流式细胞仪(flow cytometry,FCM)是一种对液相中分散着的细胞进行定性、定量分析与分选的设备,具有分析速度快、敏感性好,和精确度高的特点,能够对于不同细胞发生凋亡进度不同的过程,进行准确检测。当待检测的细胞随着液流系统经过探测点,检测到的前向散射光强度代表了细胞的大小,而侧向散射光反应细胞内颗粒的复杂程度。细胞凋亡时,细胞固缩,体积变小,细胞内颗粒往往增多,故凋亡细胞的前向散射光降低,侧向散射光增高;而坏死细胞的前向散射光和侧向散射光同时增高。因此,可区分正常、坏死和凋亡细胞。FCM可以配合荧光染料进行多参数测定,凋亡检测中常用的是AnnexinV-FITC/PI双荧光标记,能够进行早、中期凋亡阶段凋亡率的测定。 三、细胞凋亡的DNA片段检测 DNA断裂是细胞凋亡最显著的生物化学特点,细胞凋亡时,核酸内切酶与相关蛋白水解酶被激活,将DNA降解,形成长度为180~200bp或其整倍数的
(完整)常见细胞凋亡检测的方法与注意事项 编辑整理: 尊敬的读者朋友们: 这里是精品文档编辑中心,本文档内容是由我和我的同事精心编辑整理后发布的,发布之前我们对文中内容进行仔细校对,但是难免会有疏漏的地方,但是任然希望((完整)常见细胞凋亡检测的方法与注意事项)的内容能够给您的工作和学习带来便利。同时也真诚的希望收到您的建议和反馈,这将是我们进步的源泉,前进的动力。 本文可编辑可修改,如果觉得对您有帮助请收藏以便随时查阅,最后祝您生活愉快业绩进步,以下为(完整)常见细胞凋亡检测的方法与注意事项的全部内容。
常见细胞凋亡检测的方法与注意事项 大家常把细胞凋亡和细胞坏死混淆,其实两者是不同的细胞死亡形式,大家可以在死亡细胞的形态、生化和分子指标上将二者区分开来,细胞凋亡检测的方法不少,这里就总结下几种常用的检测方法. 细胞凋亡检测更多详情,点击查看不可不知的细胞检测方法——MTT 一、细胞凋亡的形态学检测 根据凋亡细胞固有的形态特征,人们已经设计了许多不同的细胞凋亡形态学检测方法。 1 光学显微镜和倒置显微镜 (1) 未染色细胞:凋亡细胞的体积变小、变形,细胞膜完整但出现发泡现象,细胞凋亡晚期可见凋亡小体。 贴壁细胞出现皱缩、变圆、脱落. (2)染色细胞:常用姬姆萨染色、瑞氏染色等.凋亡细胞的染色质浓缩、边缘化,核膜裂解、染色质分割 成块状和凋亡小体等典型的凋亡形态。 2 荧光显微镜和共聚焦激光扫描显微镜 一般以细胞核染色质的形态学改变为指标来评判细胞凋亡的进展情况。 常用的DNA特异性染料有:HO 33342 (Hoechst 33342),HO 33258 (Hoechst 33258), DAPI。三种染料与DNA的结合是非嵌入式的,主要结合在DNA的A-T碱基区。紫外光激发时发射明亮的蓝色荧光。 Hoechst是与DNA特异结合的活性染料,储存液用蒸馏水配成1mg/ml的浓度,使用时用PBS稀释成终浓度为2~5mg/ml。 DAPI为半通透性,用于常规固定细胞的染色。储存液用蒸馏水配成1mg/ml的浓度,使用终浓度一般为0.5 ~1mg/ml。 结果评判:细胞凋亡过程中细胞核染色质的形态学改变分为三期:Ⅰ期的细胞核呈波纹状(rippled)或呈折缝样(creased),部分染色质出现浓缩状态;Ⅱa期细胞核的染色质高度凝聚、边缘化;Ⅱb期的细胞核裂解为碎块,产生凋亡小体(图1)。 3 透射电子显微镜观察 结果评判:凋亡细胞体积变小,细胞质浓缩。凋亡Ⅰ期(pro—apoptosis nuclei)的细胞核内染色质高度盘绕,出现许多称为气穴现象(cavitations)的空泡结构(图2);Ⅱa期细胞核的染色质高度凝聚、边缘化;细胞凋亡的晚期,细胞核裂解为碎块,产生凋亡小体。 图2
题目:秀丽线虫生殖细胞凋亡检测 一.实验目的: 1.掌握检测凋亡细胞的方法 2.学习使用荧光染料活体染色的方法和步骤 二.实验原理 1.秀丽隐杆线虫(Caenorhabditis elegans):是一种无毒无害、可 以独立生存的线虫。其个体小,成体仅 1.5mm长,为雌雄同体(hermaphrodites),雄性个体仅占群体的0.2%,可自体受精或双性生殖;在20℃下平均生活史为3.5天,平均繁殖力为300-350个;但若与雄虫交配,可产生多达1400个以上的后代。1976年,Sulston和Horvitz利用秀丽隐杆线虫(Caenorhabditis elegans)研究发现,其约13%的体细胞在胚胎发育中注定死亡,使得人们认识到细胞凋亡的遗传基础。 2.荧光染料活体染色:本实验使用吖啶橙(Acridine orange)作为 染色剂,该染料对细胞具有慢性毒性,致癌性强,由于凋亡细胞因DNA片段化可结合更多染料,荧光显微镜下呈亮绿色,可在荧光显微镜下快速方便的检测出,适用于多数品系。 三.实验材料及设备
1.实验材料: a)各品系秀丽隐杆线虫:N2(实验组), ced-1::gfp(方法对照组),ced- 3(阴性对照) b)OP50 c)M9培养基 d)NGM培养基 2.实验设备: a)普通光学显微镜 b)载玻片若干,盖玻片若干,铂金丝 c)暗箱 d)吸水纸、滴管等 e)荧光显微镜 四.实验方法及步骤 1.线虫接种、同步化 2.取样:在12孔板培养板上,每孔吸取900μL预先接入少量OP50 的M9培养基,每孔用铂金丝挑取培养20~30条成体线虫 3.染色:向N2与ced-3品系中每孔加入250μg/mL吖啶橙100μL, 混匀后置于培养箱(避光)染色45~60min。 4.方法对照组观察:向ced-1::GFP品系中加入1滴盐酸左旋咪唑, 麻痹线虫后在荧光显微镜下观察。
细胞凋亡与坏死是两种完全不同的细胞凋亡形式,根据死亡细胞在形态学、生物化学和分子生物学上的差别,可以将二者区别开来。细胞凋亡的检测方法有很多,下面介绍几种常用的测定方法。 一、细胞凋亡的形态学检测 根据凋亡细胞固有的形态特征,人们已经设计了许多不同的细胞凋亡形态学检测方法。 1 光学显微镜和倒置显微镜 (1)未染色细胞:凋亡细胞的体积变小、变形,细胞膜完整但出现发泡现象,细胞凋亡晚期可见凋亡小体。 贴壁细胞出现皱缩、变圆、脱落。 (2)染色细胞:常用姬姆萨染色、瑞氏染色等。凋亡细胞的染色质浓缩、边缘化,核膜裂解、染色质分割 成块状和凋亡小体等典型的凋亡形态。 2 荧光显微镜和共聚焦激光扫描显微镜 一般以细胞核染色质的形态学改变为指标来评判细胞凋亡的进展情况。 常用的DNA特异性染料有:HO 33342 (Hoechst 33342),HO 33258 (Hoechst 33258), DAPI。三种染料与DNA的结合是非嵌入式的,主要结合在DNA的A-T碱基区。紫外光激发时发射明亮的蓝色荧光。 Hoechst是与DNA特异结合的活性染料,储存液用蒸馏水配成1mg/ml的浓度,使用时用PBS稀释成终浓度为2~5mg/ml。 DAPI为半通透性,用于常规固定细胞的染色。储存液用蒸馏水配成1mg/ml的浓度,使用终浓度一般为0.5 ~1mg/ml。 结果评判:细胞凋亡过程中细胞核染色质的形态学改变分为三期:Ⅰ期的细胞核呈波纹状(rippled)或呈折缝样(creased),部分染色质出现浓缩状态;Ⅱa期细胞核的染色质高度凝聚、边缘化;Ⅱb期的细胞核裂解为碎块,产生凋亡小体(图1)。 3 透射电子显微镜观察 结果评判:凋亡细胞体积变小,细胞质浓缩。凋亡Ⅰ期(pro-apoptosis nuclei)的细胞核内染色质高度盘绕,出现许多称为气穴现象(cavitations)的空泡结构(图2);Ⅱa期细胞核的染色质高度凝聚、边缘化;细胞凋亡的晚期,细胞核裂解为碎块,产生凋亡小体 二、磷脂酰丝氨酸外翻分析(Annexin V法) 磷脂酰丝氨酸(Phosphatidylserine, PS)正常位于细胞膜的内侧,但在细胞凋亡的早期,PS可从细胞膜的内侧翻转到细胞膜的表面,暴露在细胞外环境中(图3)。Annexin-V是一种分子量为35~36KD的Ca2+依赖性磷脂结合蛋白,能与PS高亲和力特异性结合。将Annexin-V 进行荧光素(FITC、PE)或biotin标记,以标记了的Annexin-V作为荧光探针,利用流式细胞仪或荧光显微镜可检测细胞凋亡的发生。 碘化丙啶(propidine iodide, PI)是一种核酸染料,它不能透过完整的细胞膜,但在凋亡中晚期的细胞和死细胞,PI能够透过细胞膜而使细胞核红染。因此将Annexin-V与PI匹配使用,就可以将凋亡早晚期的细胞以及死细胞区分开来。